Pituitary Gland (Hypophysis)
Category : 11th Class
Pituitary is known as hypophysis cerebri, its name pituitary was given by Vesalius. Muller’s gland of amphioxus and subneural gland of hardmania is homologous to pituitary of vertebrates. Weight of pituitary is 0.5 gm. Removal of pituitary is knows as hypophysectomy.
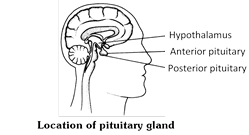
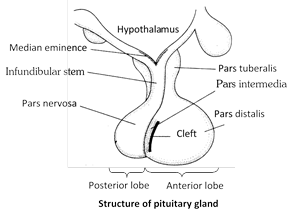
Position and origin : Pituitary gland is the smallest (about 1 to 1½ cm in diameter) endocrine gland of the body. It is pea-shaped, ovoid, radish brown gland situated at the base of the brain in a cavity, hypophyseal fossa of the sella turcica of sphenoid bone. It is connected by a short stalk called Infundibulum, to the ventral wall (Hypothalamus) of diencephalon. That is why it is also called hypophysis cerebri. It weight about 0.5 to 1 gm. It control most of the endocrine glands. Hence, it is also called leader of endocrine orchestra or master gland. Pituitary gland is closely related with hypothalamus, hence, it is also called hypothalamo-hypophyseal gland, pituitary is ectodermal in origin.
Parts and component
Adenohypophysis
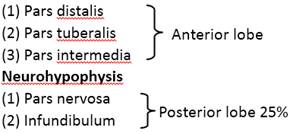
Structure of pituitary gland : Pituitary gland is comprised of two main lobes – Adenohypophysis and Neurohypophysis. Adenohypophysis is arises as hypophysial or Rathke's pouch from dorsal wall of embyronic stomodeum. It is the anterior lobe of pituitary. The neurohypophysis (Pars nervosa or Posterior lobe) form as an outgrowth from the infundibulum of the floor of hypothalamus.
In pituitary following types of cells are found :
(1) Chromophobes cells : Found in adenohypophysis of pituitary. These are not stained by acid and base dye. Pigment granules are absent. These are colourless may change into chromophils.
(2) Chromophil cells : Found in adenohypophysis of pituitary. These are stained by acid and base dye. Pigment granules are filled in these cells. These may be two types :
(i) Acidophils : It is also known as a-cells synthesize and secretes growth hormone and prolactin.
(ii) Basophils : It is also known as cyanophils or b-cells synthesize and secretes TSH, ACTH, FSH, LH and MSH hormones.
(3) Pituicyte cells : These cells found in neurohypophysis of pituitary. These are supporting neuroglia cells and gives support to herring bodies.
(4) Herring bodies : Herring bodies Are dilated terminal portion of Neurosecretory axon constituting hypothalamohypophyseal tract. They are hormone precursors for oxytocin and vasopressin.
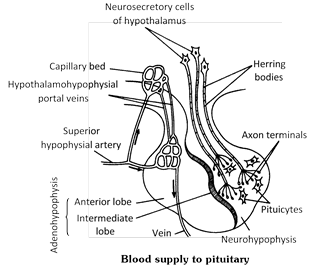
Blood supply to pituitary or Hypophyseal portal system : A pair of posterior hypophysial arteries and a pair of anterior hypophysial arteries provide blood to the pituitary gland. Posterior arteries supply blood to the pars nervosa, and anterior arteries supply blood to the hypothalamus and pars distalis. Adenohypophysis has dual blood supply by means of a "circle of willis". The anterior hypophysial artery which bring blood into this circle big ureates in to two branches outside the lobe. One branch supplies the adenohypophysis and other supplies the hypothalamus. The veins that drain the blood from hypothalamus. Then run into the pars distalis through pars tuberalis and divide into capillaries. Those veins are therefore, called portal hypophysial veins. These constitute a hypothalamo hypophysial portal system. Hypothalamic hormone reached anterior pituitary by portal system.
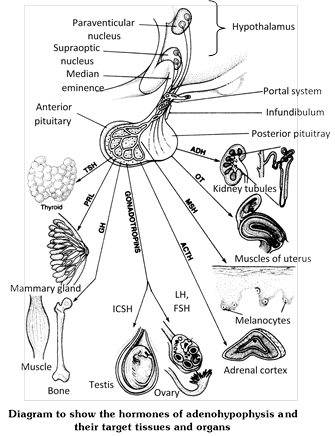
Hormones of adenohypophysis
Adenohypophysis secretes seven hormones which are proteinous in nature. These hormones controlled by the controlling factors. Secreted by the hypothalamus. These are 9 main controlling factors. Out of them 7 are releasing factors (RF) and 3 are inhibiting factor (IF). Complete failure of adenohypophysis (ant. pituitary) is leads to simmonds syndrome. Hormones that influence another endocrine gland are called tropic or tropin hormones. The FSH/LH regulate Testes and ovaries, thyrotropin stimulate thyroid, whereas corticotropin act on cortex of adrenal gland. Various hormones of adenohypophysis are as follows -
(1) Somatotropin (STH) or Growth Hormone (GH)
(i) Functions of growth hormone : Molecules of this hormone are polypeptides of 191 amino acid monomers. It is the major hormone in the secretion of anterior pituitary. It is the most important stimulant of proper normal growth of body. It promotes biosynthesis of DNA, RNA and proteins in all body cells. thus, it acts as an anabolic growth factor. Obviously, it stimulates cellular growth and proliferation, growth and repair of bones, muscles and connective tissue. In the liver cells it promotes, glycogenesis, deamination and gluconeogenesis.
According to modern scientists, the anabolic effects of growth hormone in man are indirect, instead of being direct. This hormone triggers synthesis of certain special, insulin-like growth factors (IGFs) in cells of many tissues, such as liver, muscles, cartilages, bones, etc. These growth factors are called somatomedins.
(ii) Control of the secretion of growth hormone : Secretion of growth hormone is controlled by two hormonal factors secreted by cells of hypothalamus. One of these factors, called GH-release hormone (GHRH) promotes secretion of growth hormone, while the other called GH-inhibatory hormone (GHIH) retards the secretion of growth hormone by the anterior pituitary. GHRH is also called somatocrinin and GHIH is called somatostatin.
(iii) Effects of hyposecretion of growth hormone
(a) Nanism or ateliosis : Hyposecretion (undersecretion) of growth hormone is childhood results into a blunted growth of body. Growth of all organs is retarded. Growth of bones at their epiphysial ends stops. Hence, the bones do not grow in length, so that the body remains a dwarf. This pituitary dwarfism is called nanism or ateliosis.
(b) Midgets : Unlike the thyroid cretinism, the development of brain is normal in pituitary dwarfs, but like thyroid cretinism, the pituitary dwarfs are also infertile. The dwarfs of circuses are pituitary dwarfs. these are called midgets.
(c) Pituitary myxoedema : Undersecretion of growth hormone during adolescence (between 13 to 22 years of age) restricts body height, so that the person remains short-statured. Undersecretion after growth period (about the age of 22) causes pituitary myxoedema whose symptoms are almost similar to those of thyroid myxoedema. These include old age symptoms, such as reduced BMR and protein synthesis, graying and falling of hair, pallor and dryness of skin, reduced BP and low body temperature, insomnia, and weakness of muscles, vision and wisdom. Due to accumulation of mucus under the skin, the body becomes puffy, but weak. Genitalia weaken, causing sexual disability. Hence, the person becomes disheartened.
(iv) Effects of hypersecretion of growth hormone
(a) Proportionate gigantism : Hypersecretion (oversecretion of growth hormone during growth period (childhood and adolescence) causes excessive growth (hypergrowth) of all body parts, resulting into a symmetrically giant body. This is called proportionate gigantism.
(b) Disproportionate gigantism or acromegaly : The concerned person may attain a height of 8 feet or ever more. Oversecretion of growth hormone after growth period also causes gigantism, but in this the long bones do not grow in length due to closed epiphyseal plate at their ends, but the bones of hands, feet, lower jaw and rib cage thicken. Simultaneoulsy, eyelids, lips, tongue, nose, chin, etc also enlarge. Soles, palms and forehead become wrinkled. Skin thickens and becomes wrinkled. Skin thickens and becomes coarse and fluffy (hirsutism). Consequently, the body becomes ugly like a gorilla. This is called disproportionate gigantism or acromegaly. It is common in men and rare in women.
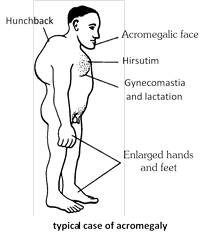
(c) Kyphosis : In some cases, the backbone bends and thickens, causing hunchback condition (kyphosis). Breasts enlarge and mammary gland may yield milk. The patients often complain of headache, sexual disorders, muscular pain, and impaired vision and memory.
(d) Hypersecretion of growth hormone raises blood glucose level (hyperglycemia) which may cause diabetes mellitus.
(e) Ketosis : Increased breakdown of fat may release ketone bodies, mainly acetoacetic acid, in blood, causing ketosis.
(2) Prolactin (PRL), Lactogenic, Luteotropic (LTH), or Mammotropic (MTH) Hormone : It is secreted by the lactotroph cells of anterior pituitary. Its molecules are polypeptides of 198 amino acid monomers. Its secretion by anterior pituitary is enhanced by prolactin-release hormone (PRH) and suppressed by prolactin inhibitory hormone (PIH) of hypothalamus. PIH is also called dopamine. In humans, it may act as a mild growth hormone, but its main physiological effect is to activate growth of breasts during pregnancy and secretion of milk by mammary glands after childbirth. That is why, it is often referred to as "maternity hormone". In some other mammals, and probably in women also, it stimulates corpus luteum of ovaries to continue secreting progesterone, hormone during pregnancy. Prolactin levels rises during pregnancy due to PRH of hypothalamus.
Hypersecretion : (i) Prolactin hormone is secreted both in males as well females. In males it influence sexual behaviour. Its hypersecretion may hinder menstruation.
(ii) May cause impotency
(iii) In pigeons and doves, it stimulates the epithelial cells of crop in both males and females to secrete "pigeon milk" for nutrition of newly hatched infants.
(3) Follicle-stimulating hormone (FSH) or Gametokinetic factor : It is a glycoprotein whose molecules consists of a polypeptide of 204 amino acid residues. It stimulates growth of seminiferous tubules and spermatogenesis in men, and growth of ovarian follicles and oogenesis in women. In women, it also stimulates secretion of female sex hormones (estrogens) by the cells of ovarian follicles. Under the negative feedback regulation, the principal male (testosterone) and female (estradiol) hormones retard secretion of FSH. In women, the effect of FSH on ovaries considerably decreases after the age of 40. Consequently oogenesis, secretion of estrogens and mestruation decline and ultimately stop. Termination of mesntruation is called menopause. GnRH (gonadotropin-releasing hormones) from hypothalamus stimulats FSH release. There is no gonadotropin inhibing hormone.
(4) Luteininzing hormone (LH), or Interstitial cell-stimulating hormone (ICSH) : This is also a glycoprotein whose molecules contain a polypeptide of 204 amino acid residues. In men it stimulates the growth and function of the interstitial cells of testes (cells of Leydig), which secrete the male hormones (androgens) to regulate the development of secondary sexual characteristics. In women, it stimulates the last stages of oogenesis, ovulation, development of corpus luteum and secretion of progesterone by the corpus luteum. Secretion of LH, like that of FSH is controlled by gonadotropin-releasing hormone (GnRH).
Both FSH and LH are secreted by the gonadotroph cells of anterior pituitary. Since both of these stimulate growth and activities of gonads, these are called gonadotropic hormones. These also activates the accessory genital organs. Secretion of these hormones begins only two to three years before puberty (age of sexual maturity - 12 to 14 years). Obviously their secretion is initiated by a "Genetic biological clock", located in hypothalamus. Further, the secretion of FSH in women are also regulated by a "Clock", located hypothalamus. Further, the secretion of FSH in women are also regulated by a "Clock of menstrual cycle". Under the regulation of both these clocks a gonadotropin-release hormone (GnRH) is secreted by hypothalamus and influences the activities of pituitary gonadotroph cells. Synthetic hormones of this category and their antagonists are now used to respectively activate or retard the activities of gonads.
(5) Adrenocorticotropin or Adrenocorticotropic hormone (ACTH) : It is secreted by corticotroph cells of anterior pituitary. Its molecules are 39 amino acid polypeptides. Its secretion or prompted by a corticotropin-release hormone (CRH) of hypothalamus. Its role is to intensity synthesis of adrenal cortical hormones, particularly the glucocorticoids. Secretion of ACTH is stimulated by low blood level of glucose, shock conditions and presence of a compound called interleukin-1 (IL-1) secreted by macrophages. Under a direct negative feedback regulation, the concentrations of glucocorticoids in blood affect the secretion of both ACTH and CRH. Hyposecretion of ACTH leads to rheumatic arthritis.
(6) Thyrotropin or Thyroid-stimulating hormone (TSH) : It is also a glycoprotein secreted by thyrotroph cells of anterior pituitary. The polypeptide of its molecule has 201 amino acid residues. Its secretion is stimulated by a hypothalamic thyrotropin-release hormone (TRH). It promotes growth and function of thyroid gland. Under the negative feedback regulation, the secretion rate of hypothalamic TRH depends on blood levels of TSH, thyroxine and glucose, and on metabolic rates of body cells. There is no thyrotropin-inhibiting hormone.
(7) Melanocyte-stimulating hormone (MSH) or Melanotropin : It was formerly called intermedin secreted by pars intermedia. This may be the condition in other vertebrates, but in humans, it is secreted by remnant cells of this lobe, which become a part of pars distalis. Its molecule is a small peptide of 13 amino acid residues. Its secretion is controlled by hypothalamic hormones, viz MRH (Melanocyte releasing hormone) and MIH (Possibly oxytocin is released at this time by posterior pituitary of both mother and the fetus. At actual Melanocyte inhibiting hormone). In lower vertebrates, the target cells of this hormone are the melanophores. Melanin is antagonistic to melanocyte stimulating hormone MSH affects spreading of the melanin granules in these cells so that skin colour darkens in fish and amphibian but in birds and mammals of the role of MSH in uncertain. In man, presence of MSH receptor in brain suggests its may influence brain activity.
(8) Metabolic hormone (MH) : It influence carbohydrate and fat metabolism of body. The hormone which influence carbohydrate metabolism is known as diabetogenic hormone. The hormone which influence fat metabolism is known as ketogenic hormone.
Hormones of neurohypophysis and their functions
The herring bodies of neurohypophysis contain two hormones - vasopressin and oxytocin - which are released from axon terminals by exocytosis and diffuse into adjacent blood capillaries when needed. These are secreted by paraventricular nucleus and supra-optic nucleus respectively. Both vasopressin and oxytocin are proteinous in nature.
(1) Vasopressin : The principal role of this hormone is to promote reabsorption of water from the distal convoluted tubules of nephrons and collecting ducts reducing excretion of water in urine (diuresis). That is why, it is also called antidiuretic hormone (ADH). Its release into blood is controlled by an "osmoregulatory centre" located in hypothalamus. Another effect of vasopressin is to increase blood pressure by contracting blood vessels (vasoconstriction) in several tissues; hence the name vasopressin.
(i) Vasoconstriction of the blood vessels of skin by this hormone retards secretion of sweat glands.
(ii) It also stimulates contraction of intestinal smooth muscles.
(iii) When vasopressin is released in excessive amounts, the urine becomes concentrated and blood is diluted, increasing BP. The osmo-regulatory centre, then, issues motor impulses to check release of vasopressin.
(iv) When vasopressin is released in smaller amounts, diuresis increases; urine becomes diluted and blood becomes concentrate, amounts, diuresis increase; urine becomes diluted and blood becomes concentrated, decreasing BP.
(v) In acute diuresis, quantity of urine may increase to about 20 litres instead of normal 1 to 2 litres per day. This condition is called polyurea or diabetes insipidus (passing of water; tasteless urine). It causes dehydration of body and thirst.
(2) Oxytocin (Child birth hormone) : This hormone stimulates contraction of uterine muscles, inducing labour pains for child birth (parturition) when secretion of progesterone hormone from the placenta declines, making the end of pregnancy. As the sensory impulse of increasing labour pain reaches hypothalamus, more and more oxytocin is released from posterior pituitary under a positive feedback regulationchildbirth, it dilates the cervix (vaginal stretching). After childbirth, it helps in normalization of the uterus and contracts breast muscles and lactic ducts to facilitate release of milk (lactation) during sucking oxytocin stimulates milk ejection so has a galactogogic effect.
Master gland : As is clear from above account, the pituitary gland plays most important regulatory role in the body. Besides regulating growth, sex and general behaviour, it also regulates the secretory activities of other principal endocrine glands and cells. Most appropriately, therefore, pituitary has been referred to as "The Master Gland" of body, or the "Chief Executive of Endocrine System", or "The Leader of Endocrine Orchestra".
Summary of the Principal Action of Anterior Pituitary Hormones
|
Hormone and Target Tissues |
Principal Action |
Hormone and Target Tissues |
Principal Action |
|
Human growth hormone (hGH) or somatotropin
|
Stimulates liver, muscle, cartilage, bone, and other tissues to synthesize and secrete insulin like growth factor of body cells, protein synthesis, tissue repair, glucose concentration. |
Prolactin (PRL)
|
Together with other hormones, promotes milk secretion by the mammary glands.
|
|
Thyroid-stimulating hormone (TSH) or thyrotropin
|
Stimulates synthesis and secretion of thyroid hormones by thyroid gland. |
Adrenocorticotropic hormone (ACTH) or corticotropin
|
Stimulates secretion of glucocorticoids (mainly cortisol) by adrenal cortex. |
|
Follicle-stimulating hormone (FSH)
|
In females, initiates development of oocytes and induces ovarian secretion of estrogens. In males stimulates testes to produce sperm. |
Melanocyte-stimulating hormone (MSH) |
Exact role in humans is unknown but may influence brain activity, when present in excess, can cause darkening of skin. |
Summary of Posterior Pituitary Hormones
|
Hormone and Target Tissues |
Control of Secretion |
Principal Actions |
|
Oxytocin (OT)
|
Neurosecretory cells of hypothalamus secrete OT in response to uterine distention and stimulation of nipples. |
Stimulates contraction of smooth muscle cells of uterus childbirth; stimulates contraction of myoepithelial cells in mammary glands to cause milk ejection. |
|
Antidiuretic hormone (ADH) or vasopressin
|
Neurosecretory cells of hypothalamus secrete ADH in response to elevated blood osmotic pressure, dehydration loss of blood volume, pain, or stress; low blood osmotic pressure, high blood volume, and alcohol inhibit ADH secretion. |
Conserves body water by decreasing urine volume; decreases water loss through perspiration; raises blood pressure by constricting arterioles. |
You need to login to perform this action.
You will be redirected in
3 sec
