Adrenal Gland
Category : 11th Class
Adrenal gland was first reported by Eustachius.
Origin and position : The adrenals are paired glands placed on the top or superior of the kidneys as cap. Hence, they are also called suprarenal glands.
Adrenals have a dual origin, they are originated from ectoderm and mesoderm both. Like thyroid, adrenals also highly vascular in nature.
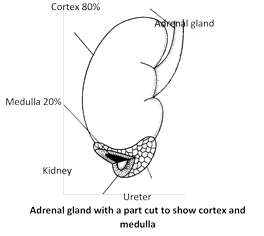
Structure : Each adrenal is a small ( 5 cm long, 3 cm broad and 1 cm thick), triangular and yellowish cap like structure. Its weight in humans is about 3.5 to 5.09 gm. At birth Adrenal gland best developed. Each gland has two parts – Outer cortex and inner medulla.
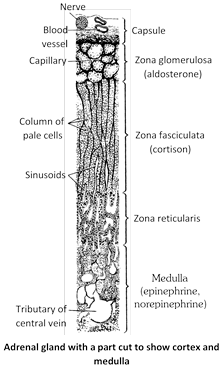
(1) Outer cortex : The cortex is derived from mesoderm and forms about 80% part of the gland. Cortex consists of fatty, cholesterol rich cells. These cells distinguish the cortex into three zones or regions.
(i) Zona glomerulosa : It is the outer part of the cortex (15% of the gland), which consists of small polyhedral cells. It secrets mineralocorticoids e.g., Aldosterone.
(ii) Zona fasciculata : It is the middle part of the cortex (50% of the gland). Which consists of large polyhedral cells. This part secrets gluco-corticoids. e.g., Cortison, Corticosterone.
(iii) Zona Reticularis : It is the inner part of the cortex (7% of the gland). In which the parallel cell cords of the zona fasciculata branched to form a loose anastomosing network. It secrets sex hormones.
(2) Inner medulla : The medulla is derived from ectoderm and forms about 20% part of the gland. Adrenal medulla is reddish brown in colour and colourless of rounded groups of short cords of relatively large and granular cells. These cells are modified postganglionic cells of sympathetic nervous system. These are called chromaffin cells or phaeochromocytes. Adrenal medulla secrets adrenalin and nor-adrenalin which are collectively called as catecholamines.
Hormones of adrenal cortex
About 20 steroids (steroidogenic) compounds have secreted from adrenal cortex. These are called adrenocorticoids (corticosteroids). Only few of them are biologically active as hormone. These hormones are steroid in nature. The later, however account about 80% of the secretion of adrenal cortex and are classified into three categories.
(1) Mineralo-corticoids : The principal mineralocorticoid is aldosterone. It is also called salt-retaining hormone. It promotes reabsorption of sodium ions from kidney and excretion of potassium ions in urine. It also reabsorb Cl– ions from kidney. Thus aldosterone has a important contribution in homeostasis by controling osmatic pressure of ECF (Extra cellular fluid).
Remember that doctors administer saline drip to the patients who lose excessive water and salts due to diarrhoea, cholera, etc. Aldosterone also helps in maintaining acid-base equilibrium and blood pH (7.35) by promoting reabsorption of \[HC{{O}^{}}_{3}\] and regulating excretion of \[{{H}^{+}}\]by kidneys. It also promotes absorption of water and salt in intestine, mainly in colon. The Renin-angiotensin-aldosterone or RAA pathway controls secretion of Aldosterone.
(2) Gluco-corticoids : These include three main hormones – cortisol, corticosterone and cortisone. Cortisol is most abundant (about 95%) and most important. These hormones play an important role in carbodydrate, fat and protein metabolism as follows -
(i) Cortisol retards glucose consumption and protein synthesis, but promotes breakdown of proteins and fats in the cells.
(ii) Effects of glucocorticoids upon liver are anabolic. These promote intake of glucose, FFAs and amino acids by cells of liver. Then, these intensify deamination of amino acids, synthesis of urea, synthesis of glucose from fatty acids and amino acids (gluconeogenesis), and synthesis of glycogen from glucose (glycogenesis) in liver cells.
(iii) Cortisol is anti-inflammatory. It retards the migratory movements and phagocytic activities of white blood corpuscles (WBCs), suppressing "inflammation reactions" which constitute the normal defense mechanism of body against toxic substances. Simultaneously, it reduces the number of mast cells, reducing secretion of histamine. This is also an anti-inflammatory effect. It also denotes synthesis of collage fibres which usually form at the sites of inflammation in normal defense. That is why, cortisol is usually injected as a drug for treatment of diseases that are caused by deposition of collagen fibres, such as arthritis or rheumatism.
(iv) Cortisol is also "immunosuppressive". It suppressess synthesis of antibodies, retarding the normal immune reactions of body against antigens and attack of micro-organisms. In fact, it induces atrophy of thymus gland and other lymphoid tissues, so that the productions of lymphocytes is inhibited. That is why, it is used for treatment of allergy. Also, it is used in transplantation surgery to suppress the formation of antibodies in the body of recipients so that the latter may accept the transplanted organs.
(v) Cortisol increases RBC count, but decreases the WBC count of blood. It also elevates blood pressure (BP).
Sex hormones : The zona reticularis of adrenal cortex secrets androgen and estrogen in small quantity. These hormones regulates the development of sex organs, secondary sexual characters and promote growth and protein metabolism.
Role of adrenal cortex in stress reaction : Adrenal glands provide the body with an emergent "chemical defence mechanism" in stress conditions that threaten the physical integrity and chemical constancy of the body. After the "Fight or Flight" reaction, the body remains in a state of shock for some time just like a country after a war. Heartbeat, cardiac output, blood pressure and glucose and salt concentrations in ECF considerably go down in this "shock condition". For example, excessive bleeding in an accidental injury immediately sends the body into shock condition. the injured must be made to recline and his / her legs must be elevated by putting a few pillows under the feet and hips. This increases venous flow of blood towards the heart, so that the cardiac output is maintained.
Whereas the hormones of adrenal medulla elevate \[{{O}_{2}}\] consumption, BMR, respiration and tension to increase alertness and responsivity to prepare the body for violent stress-reactions, those of adrenal cortex, particularly aldosterone and cortisol, serve to maintain the body in living condition and recoup it from the severe after-effects of stress reactions. An increased output of cortisol is actually "life-saving" in shock conditions. It inhibits the normal defence mechanisms and mobilises help from all parts of the body in order to keep the body alive.
Adrenal glands are large in fetus, but these mainly secrete sex hormones. By the time of child-birth, these become small and their secretions remain minimal for a few days after birth. Obviously, the "chemical defence system" is very weak in newly born infants. The latter can, therefore, easily succumb to stress conditions. That is why, infants are provided extra care in maternity homes.
As is clear from above account, adrenal cortex is very necessary for survival, but adrenal medulla is not so necessary, because its deficiency can be compensated by sympathetic nervous system.
Control of adrenal cortex secretions : Secretion of glucocorticoids and sex hormones by adrenal cortex is regulated by a hormone, corticotropin or adrenocorticotropic hormone (ACTH), secreted by the anterior lobe of pituitary gland. Secretion of ACTH from pituitary is, in turn, regulated by a "corticotropin-release hormone (ACTHRH)" of hypothalamus. A "feedback control mechanism" operates between hypothalamus, pituitary and adrenal cortex. A decrease in cortisol level in blood stimulates the hypothalamus and pituitary. Hence secretion of ACTHRH from hypothalamus and of ACTH from pituitary and, therefore, of glucocorticoids and sex hormones from adrenal cortex increases. When cortisol level in the blood rises, the control mechanism operates in reverse direction. This "feedback control" is very efficient and quick.
Secretion of mineralocorticoids is only nominally under the control of ACTH. Although adrenal glands themselves regulate secretion of mineralocorticoids according to \[N{{a}^{+}},\] water and \[{{K}^{+}}\] levels in ECF, by feedback, but this regulation is mainly provided by the kidneys. As the blood pressure goes down due to decreased amount of salt and water in blood, certain cells of afferent arterioles that supply glomeruli secrete an enzyme named renin.
Hormones of adrenal medulla
The chromaffin cells of adrenal medulla synthesize two hormones adrenalin or epinephrine (80%) and nor-adrenalin or nor-epinephrine (20%). These hormones are proteinous in nature and derived from amino acid tyrosine. Which is first hydroxylated and decarboxylated to form dopamine and than the latter is hydroxylated again to finally form norepinephrine. Epinephrine is derived by methylation of norepinephrine.
\[\text{Tyrosine }\underset{\text{Decarboxylation}}{\mathop{\xrightarrow{\text{Hydroxylation}}}}\,\text{Dopamine }\xrightarrow{\text{Hydroxylation}}\text{ }\]
\[\text{Nor epinephrine }\xrightarrow{\text{Methylation}}\text{ Epinephrine}\]
Cortisol from adrenal cortex induce synthesis of enzymes needed to convert nor epinephrine to epinephrine. Norepinephrine lacks the converting enzymes. Because the ANS controls the chromaffin cells directly, hormones release can occur very quickly.
The molecular structure of dopamine, norepinephrine and epinephrine, includes a 6-carbon ring connected to two hydroxyl groups \[(-OH).\] This is called catechol ring, and these compounds are called catecholamines for this reason.
Epinephrine (adrenalin) was first extracted by Abel (1899) who coined this name for it. It was, however, extracted in pure form by Jokichi and Takamine (1900). Its molecular structure was worked out by Aldrich in 1901. Stolz (1904) and Dakin (1905) synthesized it in their laboratories. Norepinephrine was discovered by Ulf von Euler (1946). Effects of these hormones were studied by Axelrod (1965). For their discoveries. Euler and Axelrod won Nobel Prize in 1970.
Function of epinephrine
(1) Epinephrine causes constriction of the blood vessels (vasoconstriction) which supply blood to those peripheral and abdominal organs (skin and organs of digestive, excretory and reproductive systems) that normally remain active while we are resting or sleeping. Obviously, the activities of these organs are retarded, but the blood pressure (BP) increases.
(2) Reduced supply of blood causes a pale skin (pallor), but arrector pilli muscles of skin contract, causing gooseflesh.
(3) Mouth becomes dry due to poor secretion of saliva.
(4) Food digestion is retarded because of reduced gut peristalsis due to relaxation of the smooth muscles of gut wall, as well as, because of poor secretion of digestive glands.
(5) Kidneys produce small volume of urine, and muscles or urinary bladder relax.
(6) In pregnant women, the muscles of uterus contract, increasing the possibility of abortion.
(7) Epinephrine causes dilation of blood vessels (vasodilation) which supply brain, skeletal muscles, heart, lungs, liver, adipose tissues, sensory organs, etc. Due to increased blood supply, these organs become very active, inducing alarm reaction. Obviously, the blood pressure, increased due to effect of norepinephrine, is reduced to some extent.
(8) Pupils dilate due to contraction of radial dilatory muscles of iris. Secretion of tear by lacrimal glands increases.
(9) Epinephrine causes relaxation of the smooth muscles of trachea, bronchi and bronchioles. These organs, therefore dilate, so that breathing becomes easier and faster. Remember that epinephrine is used in treatment of asthma for this reason.
(10) Contractions of cardiac muscles intensify, increasing both rate and force of heartbeat, pulse rate, arterial pressure and cardiac output.
(11) Due to an increase in adhesiveness of blood platelets, the time of blood clotting is considerably reduced.
(12) The spleen contracts, releasing its reserve of blood corpuscles whose number in blood, therefore, increases.
(13) In islets of Langerhans in pancreas, secretion of insulin hormone decreases, but that of glucagon increases. Glucagon causes glycogenolysis, i.e. breakdown of glycogen into glucose in liver and skeletal muscles.
(14) Because of an increase in blood levels of O2 glucose, FFA, etc the basal metabolic rate of all body cells considerably increases and renders the whole body highly active and irritable.
(15) External genitalia become flaccid, but ejaculation becomes early and forceful.
Since the rate and force of the activities of most internal organs increase in a few seconds under the effects of epinephrine and norepinephrine, the various changes can be detected by a lie detector polygraph to ascertain the emotional state of a person.
Difference between Adrenal cortex and Adrenal medulla
|
S.No. |
Adrenal cortex |
Adrenal medulla |
|
1. |
It is external firm region of the adrenal gland. |
It is central soft region of the adrenal gland. |
|
2. |
It is pale yellowish-pink in colour. |
It is dark reddish-brown in colour. |
|
3. |
It is enclosed by a fibrous capsule. |
It is not enclosed by a fibrous capsule. |
|
4. |
It forms about 80% of the adrenal gland. |
It forms just 20% of the adrenal gland. |
|
5. |
It develops from the mesoderm. |
It develops from the ectoderm (neural crests). |
|
6. |
It consists of 3 concentric regions : Outer zona glomerulosa, middle zona fasiculata and inner zona reticularis. |
It is not differentiated into regions. |
|
7. |
It is essential for life, its destruction causes death. |
It is not essential for life, its destruction does not cause death. |
|
8. |
It secretes 3 groups of hormones : mineralocorticoids, glucocorticoides and gonado corticoids |
It secretes 2 similar hormones nor adrenaline and adrenaline. |
|
9. |
It is stimulated to release its hormones by the adrenocorticortrophic hormone from the anterior pituitray. |
It is stimulated to secrete its hormones by nerve impulses reaching via sympathetic nerve fibres. |
|
10. |
There is no cooperation between adrenal cortex and sympathetic nervous system. |
Adrenal medulla and sympathetic nervous system function as an integrated system called sympatheticoadrenal system. |
|
11. |
It causes many deficiency / excess disorders. |
It is not known to cause any disorder. |
Significance of adrenal medullary hormones
Relationship between adrenal medulla and sympathetic nervous system : Our routine in voluntary activities like food digestion, respiration, heartbeat and blood circulation, thermoregulation, peristalsis of tubular organs, secretion of glands, excretion, etc are continuously and automatically done by our internal (visceral) organs without the conscious control of our brain. These are, therefore, called involuntary activities, these activities occur under the control of autonomic nervous system and their co-ordinated regulation is controlled by the hypothalamus of brain. The autonomic nervous system controls these activities by affecting the activity levels of cardiac muscles, smooth muscles of visceral organs and blood vessels, and the glands. The autonomic nervous system comprises two control systems, having antagonistic effects of these organs. These are sympathetic and parasympathetic systems. Obviously, the motor nerve fibres of both these systems, originating from central nervous system (CNS), innervate most of the internal organs. The motor fibres of parasympathetic system stimulate those organs which remain more active while we are at rest or sleeping. contrarily, the motor fibres of sympathetic system stimulate those organs which remain more active when we are awake and doing work.
The fibres of sympathetic system, innervating the organs, the postganglionic motor fibres. At their terminals, these release norepinephrine, a neurotransmitter which triggers an alteration in the activities of concerned organs. The adrenal medulla is also innervated by fibres of sympathetic system, but these are preganglionic fibres of this system. At their terminals these fibres release acetylcholine which stimulates chromaffin cells to release their hormones – epinephrine and norepinephrine. Circulating in blood, these hormones reach into the internal organs and not only increase the effects of sympathetic stimulation, but also prolong these effects about ten-fold. That is why, the sympathetic system and adrenal medulla are collectively considered as sympathoadrenal system, and the hormones of adrenal medulla are called sympathomimetic amines. Besides this, the medullary hormones, especially epinephrine, increase the basal metabolic rate (BMR) of all body cells, increasing the activity and irritability level of whole body. Since, however, the effects of sympathetic system and adrenal medullary hormones are complementary, a retarded efficiency of any one of these is compensated by the other.
Modern scientists have discovered that cells resembling chromaffin cells occur in small groups near the thoracic and abdominal ganglia of sympathetic system. These groups have been named paraganglia.
Alarm or stress reaction : Physico-chemical changes continuously occur in the external and internal environments of our body during our daily routine life, and our body keeps on maintaining homeostasis and functional equilibrium by counteracting the effects of these changes by alterations and co-ordinated regulations of the activities of various organs by sympathetic system under hypothalamic control. However, the emergency or stress conditions such as fear, anger, intense pain, accident and injury, burning, intense cooling or heating of body, sudden invasion of micro-organisms, poisoning, emotional upsets due to insult, restlessness, mental tension, anxiety, exertion, surgery, etc tend to disturb homeostasis and functional equilibrium to such an extent that the very survival of body in endangered.
As the sensory impulses of such strong stimuli called stressors, reach the brain, directly or through spinal cord, motor impulses or required responses are issued by hypothalamus to all organs, including adrenal medulla through the spinal cord. Consequently, norepinephrine is released simultaneously in all organs by sympathetic fibres, and a large amount of both epinephrine and norepinephrine is poured into blood by adrenal medulla. This "mass release" of these hormones prepares the whole body, within seconds, for a violent physical reaction called alarm or stress reaction, and often referred to as general adaptation syndrome (GAS). In this reaction, the concerned person either boldly faces the emergency, or tries somehow to escape from it. That is why, it is called "Fight or Flight reaction".
Effects of irregularities of adrenal secretion
(1) Hyposecretion : This may be a genetic defect. Undersecretion of adrenocorticoids (hypocorticism) causes Addison's disease which is relatively rare and occurs in both men and women between the ages of 20 to 40 years. This disease was first described by Thomas Addison in 1849, 1855. It is maintained in following symptoms :
(i) Owing to low aldosterone and gluco-corticoides level in blood, considerable amount of sodium ions and water is excreted in urine, leading to dehydration, low blood pressure, and weakness, all symptoms of a peculiar, Addinosonean anaemia which is different from common pernicious anaemia resulting from entirely different causes like diarrhoea, cholera, etc.
(ii) Owing to low cortisol level, glucose level also falls in blood (hypoglycemia). This sharply reduces BMR in body cells. Due to hypoglycemia and hyperkalemia (increased \[{{K}^{+}}\] level in blood) efficiency of brain, liver, skeletal and cardiac muscles, etc declines. Body temperature also falls. Heartbeat may even stop, causing death.
(iii) Decreased cortisol level induces gastro-intestinal disorders, resulting in loss of appetite, nausea, vomiting, diarrhoea, abdominal pain and restlessness.
(iv) Due to a sharp decline in body's chemical defense and resistance, sensitivity to cold, heat, infection, poisoning and other adverse condition increases. Acute hypocorticism is catastrophic and resistance, sensitivity to cold, heat, infection, poisoning and other adverse conditions increases. Acute hypocorticism is catastrophic and threatens life. Complete destruction of removal of adrenals causes death in a short time, principally because of loss of excessive sodium in urine.
(v) Addison's disease also causes an increase in the number of WBCs, resulting into eosinophilia, lymphocytosis, leucocytosis, etc.
(vi) Undersecretion of sex hormones causes impotence in males and disorders of menstrual cycle in females.
(vii) Excessive deposists of melanin, particularly in the skin of open parts of body like face, hands, feet, neck, teats, etc cause deep bronzing of skin in these parts.
(viii) As increase in \[{{H}^{+}}\]concentration in blood may cause acidosis.
(2) Hypersecretion : Oversecretion of adrenocorticoids (hypercorticism) causes following disorders and diseases -
(i) Glucose level rises in blood (hyperglycemia). This may lead to diabetes mellitus.
(ii) Irregular deposits of fat, particularly in thoracic parts and face, imparts asymmetrical shape to the body the face becomes red and rounded (moon face), shoulders swell (buffalo humps) and abdomen dilates and often shows lines of stretching. All these are symptoms of Cushing's disease (Cushing, 1932). Patients may die from brain haemorrhage, cardiac arrest, pneumonia, etc.
(iii) Retention of sodium and water is the ECF increases blood pressure, causing severe hypertension and associated symptoms like severe headache.
(iv) Excessive loss of potassium in urine causes potassium deficiency (hypokalemia). This leads to muscular weakness and convulsions and nervous disorders, and may even cause tetany and paralysis, copious and frequent urination (polyuria) and thirst, bed urination (nocturia), etc. Similarly, excessive loss of H+ in urine may cause alkalosis.
(v) Excessive mobilization of materials from all parts of body had widespread deteriorating effects. For instance, mobilization of proteins from all cells causes tissue wasting similarly, mobilization from bones renders the bones weak and fragile (osteoporosis).
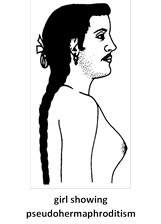
(3) Excessive secretion of male hormones (androgens) in a female fetus before complete formation of ovaries results into pseudohermaphroditism due to masculinization of external genitals, and causes abnormal development of muscles, hair on face (beard and moustache), early sexual maturation, hoarse voice and absence of menstruation. The clitoris grows to penis size, while vagina and uterus remain underdeveloped. This is known as adrenogenital syndrome. The resultant females are sterile. Oversecretion of androgens after complete formation of ovaries and fallopian tubes causes only a moderate enlargement of clitoris. Oversecretion of androgens in girls after birth causes a gradual masculinization manifested in overgrowth of clitoris, under development of mammary glands and uterus and disturbed menstruation. Oversecretion of androgens in male children causes excessive development of penis (marcogenitosomia) and other secondary sexual organs and characteristics, but atrophy of testes so that there is no spermatogenesis. Early erections are noted. Due to the anabolic effects of androgens, both in girls and body, growth is accelerated, muscles are well-developed and strong, and bones mature early.
(4) Excessive secretion of female hormones in adult males cause enlarged mammary glands (gynaecomastia) and retards growth of beard. Contrarily, excessive secretion of androgens in females in masculinizing and causes hirsutism (increased facial and body hair and muscle growth, clitorial enlargement, etc.)
You need to login to perform this action.
You will be redirected in
3 sec
