Pancreas
Category : 11th Class
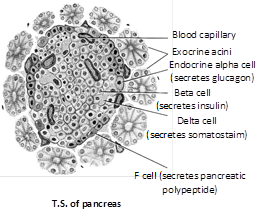
Location and origin : Pancreas (Gr. pankreas = sweet bread; Fr., pan = all + kreas = flesh) is a flattened and pinkish mixed gland (both exocrine and endocrine) situated in the concavity formed by duodenum just behind the stomach. It measures about 15 cm in length and 4 to 5 cm in breadth. It forms by fusion of two bilateral endodermal processes of embyronic intestine (duodenum of future adult).
Structure : About 99% part of the gland is exocrine and formed of hollow pancreatic acini or lobules embedded in a connective tissue stroma. In the stroma, there are numerous (approximately 1 to 2 million in human pancreas) small (0.1 to 0.2 mm in diameter) clusters of endocrine cells, called islets of Langerhans after the name of their discoverer, Paul Langerhans (1869).
Cells Types in the Pancreatic Islets
Each pancreatic islet includes four types of hormone-secreting cells :
(1) Alpha or A cells constitute about 15% of pancreatic islet cells and secrete glucagon.
(2) Beta or B cells constitute about 80% of pancreatic islet cells and secrete insulin.
(3) Delta or D cells : It’s constitute about 5% of pancreatic islet cells and secrete somatostatin (identical to growth hormone-inhibiting hormone secreted by the hypothalamus).
(4) F cells : It’s constitute the remainder of pancreatic islet cells and secrete pancreatic polypeptide.
Hormones of pancreas and their role
The \[\beta \] and \[\alpha \] cells of islets of Langerhans respectively secrete insulin and glucagon hormones which are important regulation of carbohydrate, protein and fat metabolism in the body.
(1) Insulin : In 1889, Minkowski and Mehring discovered that pancreas is related with the disease of diabetes mellitus in humans. Normal concentration of glucose in blood is about 100 mg (0.1 gm) per 100 ml. It increases somewhat after a carbohydrate rich food. Then, the secretion of insulin increases. It increases the permeability of all cells for glucose several times, except that of brain cells and red blood corpuscles (RBCs). The brain cells and RBCs are already highly permeable to glucose. After taking more glucose from blood, the cells utilize it for energy-production. Consequently, the basal metabolic rate (BMR) and RNA and protein synthesis increases in cells.
In 1923, two Canadian scientists, Banting and Best succeeded in preparing a pure extract of insulin from the pancreatic islets of a new born calf with the help of Macleod, Banting and Macleod won the 1923 Nobel prize for this work. Later, Abel (1926) succeeded in preparing pure crystals of insulin. F. Sanger (1955) worked out the molecular structure of bovine insulin and won the 1958 Nobel Prize. He discovered that insulin is a small protein whose molecule consists of two polypeptide chains, \[\alpha \]and \[\beta ,\] joined by disulphide linkages and respectively formed of 21 and 30 amino acid residues. Insulin is the first protein to be crystallized in pure form, first protein whose molecular structure was worked out, the first protein to be synthesized in laboratory in 1964, and also the first protein to be commercially manufactured by means of DNA recombinant technique. Even the human insulin was also synthesized by Tsan in 1965.
(i) Hypoinsulinism : In insulin deficiency, body cells fail to obtain glucose from blood. Hence, glucose level of blood rises, a condition called hyperglycemia. When glucose level rises further, glucose starts passing out in urine. This condition is called glycosuria. Ultimately, when glucose level in blood rises to more than 200 mg/100 ml blood the person concerned suffers from diabetes mellitus in which the urine becomes sweet.
Diabetes mellitus has been known to Greeks as a human disease since 1500 B.C. in England, it was known as a "pissing evil" due to copious urination in it. Modern scientists have discovered that diabetes mellitus is of two types - I and II. The type I diabetes is usually found in young people, in some of which it is hereditary. About 10% of diabetes patients suffer from this type. Other patients suffer from diabetes of type II, usually found in people of over 40 years of age or obesse persons. Diabetics excrete large volumes of urine. This is called polyuria. It results into dehydration which, in turn, causes increased thrist (polydipsa) and hunger (polyphagia). Being unable to utilize glucose for energy-production ("starving in midst of plenty"), the cells utilize their proteins for it, causing "body wasting". The body, therefore, becomes very weak. Nervous system may be damaged and often cataract occurs. Lipolysis in adipose tissues increases, elevating blood level of free fatty acids (FFA). Accelerated, but incomplete, oxidation of fatty acids for energy, especially in liver, results into the formation of ketone bodies - acetone, acetoacetic acid and \[\beta -\]hydroxybutyrate-, causing ketosis. Since the ketone bodies are sweet, acidic and poisonous, their increased amount in blood causes acidosis. Hence, patients may anytime become unconscious (coma condition) and finally die.
Regular injections of insulin must be given to chronic patients of diabetes. Balanced diet, exercise, and regular intake of insulin tablets (eg dionyl) may keep diabetes in control. Certain drugs, like glyburide, which stimulate insulin secretion are now available.
(ii) Hyperinsulinism : Oversecretion of insulin enhances glucose intake by most body cells and glycogenesis in liver and muscles, causing a persistent decrease in blood glucose level (Hypoglycemia) since brain cells and cells of retina and germinal epithelium mainly depend on glucose for energy, nervous efficiency, fertility and vision sharply decline. Poor supply of glucose to the brain stimulates sympathetic nervous system, causing unnecessary excitement and feeling of anxiety, sweating, weakness, fatigue and muscular convulsions. Continued excess of insulin in blood causes "coma (insulin shock)" and death. Injections of cortisol, adrenaline, growth hormone and glucagon help in treatment of hyperinulinism, because these hormones retard glucose utilization in cells and mobilize glucose and fatty acids respectively from liver and adipose tissues. Injections of glucose also give relief to the patients.
(2) Glucagon : This is secreted by the alpha cells of islets of Langerhans. It was discovered by Kimball and Murlin (1923). Like insulin, it is also a small protein. Its molecule consists of a single polypeptide chain of 29 amino acid residues. Its function is to elevate glucose level in blood when glucose is deficient. For this, glucagon intensifies glycogenolysis, deamination and gluconeogenesis, and inhibits glycogenesis in liver cells. It also intensifies lipolysis in adipose tissues. Thus, it is promoter of catabolic metabolism. When, during excessive physical labour and stress, glucose consumption in the body increases and blood glucose level falls, glucagon is secreted to normalize the glucose level.
The secretion of insulin and glucagon is regulated by a "limit-control feedback" or "push and pull feedback" control system. When sugar level in blood increases, insulin is secreted and secretion of glucagon is inhibited. When, due to the effect of insulin, blood sugar level falls, secretion of insulin is inhibited and that of glucagon is stimulated.
(3) Somatostatin and Pancreatic polypeptide : Modern physiologists have postulated that the \[\delta \] and F (PP) cells of pancreas respectively secrete somatostatin (SS) and pancreatic polypeptide (PP). Somatostatin resembles the growth hormone inhibitory hormone (GHIH) secreted by hypothalamus. Its molecule is a small peptide of 14 amino acid residues. Acting as a paracrine hormone, it serves to retard secretory activities of \[\alpha \] and \[\beta \] cells. Besides this, it also slows down food digestion, absorption of digested nutrients and assimilation of nutrients in cells. Thus, it prolongs utilization of every feed. pancreatic polypeptide (PP) also acts as a local, paracrine hormone. It retards secretion of pancreatic enzymes and somatostatin. It also inhibits motility of stomach, duodenum and gall bladder.
Difference between diabetes mellitus and diabetes insipidus
|
S.No. |
Diabetes mellitus |
Diabetes insipidus |
|
1. |
It is due to deficiency of insulin. |
It is due to deficiency of ADH. |
|
2. |
The blood sugar becomes high and glucose appears in urine. |
The blood glucose is normal and glucose does not appear in urine. |
|
3. |
There is high blood cholesterol and ketone body formation. |
There is no such phenomenon. |
You need to login to perform this action.
You will be redirected in
3 sec
