Female Reproductive System
Category : NEET
Female Reproductive System
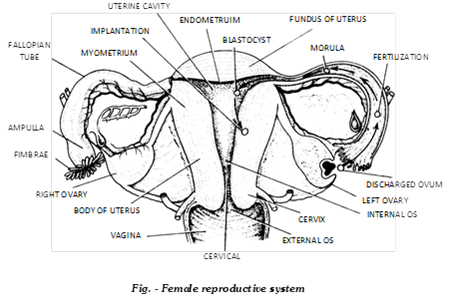
The female reproductive system consists of a pair of ovaries, a pair of fallopian tubes, uterus, vagina, external genitalia or vulva and breasts.
(i) Reproductive organ
(a) Ovaries: Ovaries are the primary sex organs of female.
(1) Size and form: The ovaries are almond shaped bodies, about 3 cm long, 1.5 cm wide and 1 cm thick.
(2) Role: The ovaries, like the tests, have both an exocrine function (production of ova) and an endocrine role (secretion of female sex hormones: estrogen and progesterone). After menopause, the ovaries become small and lose follicles.
(3) Location: Each ovary is located close to the lateral walls of the pelvic cavity, being suspended from the dorsal body wall just behind the kidney, by a section of peritonium, the mesovarium. It is held in position by several connective tissue ligaments. Each ovary is connected by an ovarian ligament to the uterus, and by a suspensory ligament to the lateral pelvic wall. It has hilus where nerves and blood vessels are connected.
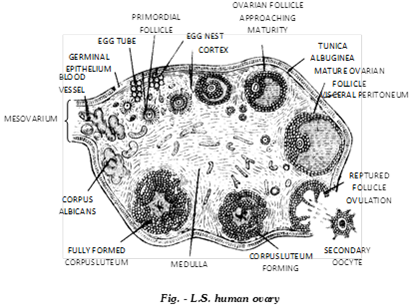
(4) Structure: Each ovary is a compact or solid organ, consisting of an outer cortex and inner medulla. The stroma of the cortical region is composed of spindle shaped fibroblasts. A poorly delineated dense connective tissue layer, the tunica albuginea, covers the cortex. It imparts the whitish colour to the ovary. Located outside the tunica albuginea, the germinal epithelium, formed of simple squamous or cuboidal epethelial cells, covers the surface of the ovary.
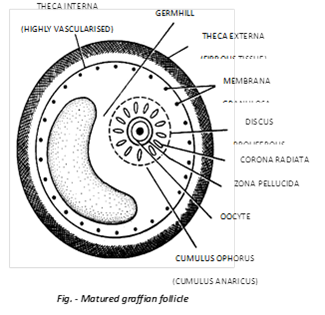
Cells of germinal epithelium give rise to groups of oogonia that project into cortex as cords called egg tubes of Pfluger, each with a round terminal mass of oogonia called egg nest. Egg nests give rise to ovarian follicles. In neonate female baby the ovary contains about 2 million follicles but 50% of them are atretic or degenerate. Atresia continues and by the time of puberty some 3,00,000 - 4,00,000 ovarian follicles are present in an ovary. However, only 450 ovarian follicloes mature, one by one alternately in the two ovaries at intervals of 28 days. A mature ovarian follicle is called Graffian follicle. It has a diameter of 10 mm. Outer fibrous theca externa and inner cellular theca internal are derived from spindle cells of cortex. Estrogen secreted by the internal theca of graffian follicle. Other constituents are follicular cells (nourishing cells formed from undifferentiated oogonia), an antrum or follicular cavity having liquor folliculi and an eccentrically placed oocyte. Follicular cells form a cellular sheath (below theca internal) called membrane granulosa and cellular mass called cumulus ovaricus covering the oocyte. Cumulus oophorus or cumulus ovaricus differentiates into outer discus proligerous and inner corona radiata. Alongwith oocyte it also secretes a mucoprotein membrane called zona pellucida. Oocyte (secondary oocyte with metaphase of meiosis II) is 50 - 100 mm. It is microlecithal (alecithal according to some workers). Oocyte membrane is called vitelline membrane. There are three coverings around the egg - inner zona pellucida, middle corona radiata and outer discus proligerous. A polar body is found between viteline membrane and zona pellucida. Graffian follicle develops under influence of FSH of anterior pituitary. Its follicular cells secrete estrogen. Estrogen brings about proliferation of lining layer of uterus, vagina and fallopian tubes. Rising level of estrogen decreases production of FSH and stimulates secretion of LH. The two cause the mature Graffian follicle to rise to the ovarian surface and burst open releasing ovum (ovulation). It occurs 10 - 14 days of mestrual cycle. The empty ruptured Graffian follicle is called corpus haemorrhagic. It usually contains a blood clot. The ruptured follicle shows proliferation of cells of membrana granulosa, deposition of yellow pigment or luteum and formation of yellow body called corpus luteum. It grown in size to about 2.5 cm. Corpus luteum secretes progesterone Ultimately corpus luteum loses its yellow colour, becomes changed to corpus albicans and then degenerates. Some thecal cells located around the follicle become active interstial cells which secrete small amount of androgen.
(b) Fallopian tubes / uterine tubes / Oviducts: Each ovary is located in front of a funnel shaped opening of the uterus, the oviduct. The oviduct is a muscular tube, measuring about 12 cm in length. Its lumen is lined by ciliated epithelium.
(1) Serosa: It is the outermost layer of visceral-peritoneum.
(2) Muscle-layer: The middle layer of the oviduct is made up of unstriped-muscle.
(3) Mucous membrane: It is the innermost layer. This layer is made up of ciliated epithelium and the connective tissue.
The oviduct shows 4 regions -
(i) Infundibulum: It is the broad, funnel-shaped proximal part. Its margin bears motile, finger-like processes called fimbriae. It opens into the body cavity by an aperture called ostium. The latter lies close to the ovary to receive the egg released from the ovary. The fimbriae bear cilia which beat toward the ostium to direct the egg into the infundibulum.
(ii) Ampulla: It is the long, wide, thin-walled, tortuous major part of the fallopian tube next to the infundibulum.
(iii) Isthmus: It is the very short, narrow, thick-walled, straight part that follows the ampulla.
(iv) Uterine part: It is also narrow and passes through the uterine wall, and communicates with the uterine cavity.
In most vertebrates both the ovaries and oviducts are functional. In birds the right ovary and right oviduct are atrophied (Degenerated). Being nonmammalian, the birds also lack mammalian sex organs and characters like uterus, external genitalia and mammary glands.
(c) Uterus
(1) Structure of uterus: It is preform, hollow muscular thick-walled but distensible median structure located above and behind urinary bladder that is meant for nourishing and development of foetus. For this uterus is capable of tremendous enlargement. The empty uterus is 7.5 cm long and 5 cm broad and 2.5 cm thick. Lining layer of uterus, called endometrium (mucous membrane), consists of an epithelium and lamina propria of connective tissue. Epithelium is a mixture ciliated and secretory columnar cells. Lamina propria contains tubular glands, fibroblasts and blood vessels.
It has four regions -
(i) Upper wide, domeshaped fundus that receives the fallopian tubes.
(ii) Cornua, the upper corners where the oviducts enter the uterus.
(iii) Middle large body or corpus which is the main part.
(iv) Lower narrow cervix that projects into the vagina. The cervix communicates above with the body of the uterus by an aperture, the internal os, and with the vagina below by an opening, the external os.
The line demarcating the body and the cervix is called isthmus. It corresponds to the internal os.
The uterus has a thick, highly vascular wall composed of three tissues: outer peritoneal covering called perimetrium, middle smooth muscle layer termed myometrium, and inner mucous membrane known as endometrium. Longest unstriped muscles of the body are found in the walls of uterus.
(2) Ant flexion: The normal position of the uterus is anteflexed, that is, it is bent forward on itself at the level of the internal os so as to lie almost horizontally over the bladder. The cervix is composed largely of the biggest and the most powerful sphincter muscle in the body. It is strong enough to hold about 7 kg. of foetus and fluid in the uterus against the pull of gravity during pregnancy.
(3) Capacity of uterus: The cavity of the uterus can expand 500 times during pregnancy, from \[10c{{m}^{3}}to\text{ }5,000c{{m}^{3}}\].
(4) Types of uterus
(i) Duplex: These are the simplest type of uteri. In it both the uteri are completely separated and open independently into the vagina through two separate openings e.g. Rat.
(ii) Biparite: In these uteri, the lower part of the two uteri are fused and there is a septa in between the two, e.g., Carnivore mammals.
(iii) Bicornuate: The lower parts of the 2 uteri are fused with each other but the partition wall is absent, e.g. Rabbit.
(iv) Simplex: When both the uteri are completely fused with each-other to form only one structure, these are the most developed uteri e.g. Man.
(5) Functions of uterus: The uterus plays multiple role. It receives the ovum from the fallopian tubes, forms placenta for the development of the foetus and expels the young one at birth.
(d) Vagina: It is tubular female copulatory organ, passageway for menstrual flow as well as birth canal of about 7 - 9 cm length between external opening (vaginal orifice) in vestibule and cervix with depression or fornix around cervix, two longitudinal ridges and numerous transverse folds or vaginal rugae. Vaginal wall is made of an internal mucosa, muscular layer and an outer adventitia. Its mucous membrane is nonkeratinised stratified squamous epithelium. Glands are absent. However, cervical glands do pass on some mucus into it during ovulation the epithelial cells contain glycogen (from puberty to menopause) which shows cyclic changes. Certain bacteria (species of Lactobacillus and Lactoneustroc, also called Doderlein's Bacillus) bring about fermentation and produce acid which inhibits growth of other microorganisms. In virgins the vaginal orifice is partially covered by an annular centrally perforate membrane called hymen.
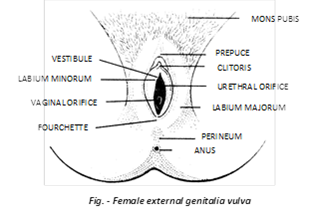
(e) External genitalia / vulva: There is a depression, the vestibule, in front of the anus. It is flanked by two pairs of fleshy folds of skin: the inner small, thin, moist, labia minora and outer larger, hair-covered labia majora. All the labial folds have numerous sebaceous and sweat glands on both sides. A small erectile organ, the clitoris, lies at the anterior junction of the labia minora. It is homologous to the penis in the male but is very small and solid, having no passage through it. It consists of a short shaft with erectile tissue. It ends in a rounded glans clitoridis. The latter is covered by a small hook of skin, the prepuce. Rubbing of clitoris during intercourse produces a pleasurable sensation. This seems to be its only function. A membranous fold, called fourchette, connects the posterior ends of the labia minora. The area between the fourchette and the anus is termed perineum. Urethra and vagina open by separate apertures, the upper urethral and lower vaginal orifices, into the vestibule. The vaginal orifice is normally covered in the virgin by a membrane, the hymen. A slit in the hymen allows menstrual flow to pass out. The hymen is ruptured during first copulation, or due to some other reason. The hymen presumably has a protective role, but is absent in many women. A fleshy elevation above the labia major is known as mons veneris or mons pubis. It bears pubic hair.
(f) Bartholins or vestibular glands: They are a pair of small glands which open in the vestibule lateral to vaginal orifice. The secretion is thick, viscid and alkaline for lubrication and counteracting urinary acidity (similar to Cowper's glands in males).
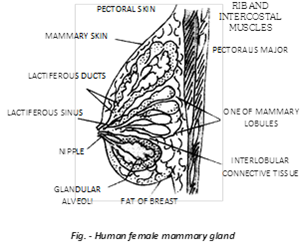
(g) Breasts / Mammary glands: The breasts are rounded eminences located over the pectoral muscles on the front wall of the thorax. These enlarge considerably in the adult female. Each breast has near its middle a nipple surrounded by a circular, pigmented (deep pink to brown) area called areola. The breasts contain fatty and connective tissues and mammary (milk) glands. The latter are compound saccular glands and are modified sweat glands. The connective tissue supports the mammary glands and the adipose tissue covers them. The glands open on the nipples, the lactiferous ducts. Just under the nipples, the lactiferous ducts widen to form lactiferous sinuses, to store milk during lactation. A nursing mother produces 1 to 2 litres of milk per day.
Rudimentary milk glands are present in the male also. Low level of estrogen in males checks the development of secretory tissue as well as fat deposits.
(ii) Onset of puberty in the females: Woman attains puberty about the age of 13. Its onset it triggered by the production of the anterior pituitary's follicle-stimulating hormone (FSH) which promotes growth of the ovarian follicles. The follicles then secrete the hormone estrogen from the follicle cells in the ovaries. This hormone brings about the growth and maturation of the reproductive tract and the development of accessory sex character. The latter include growth of breasts and external genitalia, broadening of pelvis, growth of pubic and axillary hair, increase in the subcutaneous fat, particularly in thighs, shoulders, buttocks and face to give a typical feminine contour and initiation of menstruation and ovulation.
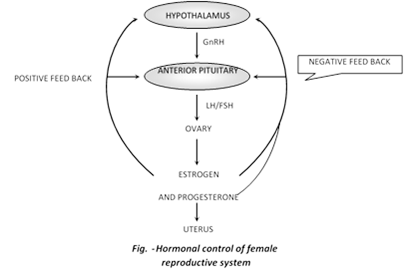
(iii) Hormonal control of female reproductive system: Ovary is regulated by pituitary gonadotropins or GnRH. Anterior pituitary secretes follicular stimulating hormone (FSH) which controls of the transformation of young primary follicle into Graffian follicle, maturation of ovum and secretion of estrogens by its follicular cells. The Luteinizing Hormone (LH) of anterior pituitary regulates the ovulation from the Graffian follicle, transformation of empty Graffian follicle into yellowish, conical corpus luteum and secretion of progesterone hormone from the corpus luteum.
Growth and function of secondary sex organs are regulated by estrogens and progesterone. Estrogens control the growth, maintenance and functioning of secondary sex organs of female. Progesterone suspends ovulation during pregnancy, promotes implantation of foetus on the endometrium and development of foetus in the uterus.
At the end of pregnancy, the corpus luteum secretes relaxin which broadens the pelvis for easy parturition.
(iv) Reproductive cycle in female: The events involved in reproduction in female mammals occur in a cyclic manner. Constituting the reproductive cycle or ovarian cycle. The reproductive cycle is of two types:
(a) Oestrous cycle (b) Menstrual cycle
Oestrous cycle: The oestrous cycle consists of a few days of oestrus or "heat" followed by a few days of anestrus of "quiescence".

(b) Menstrual cycle: The gamete formation in females is a cyclic activity that takes about 28 days and involves changes in the structure and function of the entire reproductive system. It is called menstrual cycle.
(1) Period: The length of menstrual cycle varies widely in women, but on average it is completed in 28 days (mensem means a month). In a female, successive cycles may vary in length by 1 to 2 days. It is absent during pregnancy, may be suppressed during lactation and permanently stops at menopause.
(2) Phase: Menstrual cycle is divided into four phases -
(i) Follicular (Proliferative) phase or Post-menstrual or Pre-ovulatory phase: It follows the menstrual phase and lasts for about 10 - 12 days (from 5th to 14th day of menstrual cycle). It involves following changes:
(a) Under the stimulation of FSH-RF of hypothalamus, there is increased secretion of FSH from anterior pituitary.
(b) FSH stimulates the change of a primary follicle of the ovary into a Graffian follicle.
(c) Follicular cells of Graffian follicle secrete estrogens. Estrogens have the following effects:
(1) Stimulate the growth, maintenance and normal functioning of secondary sex organs.
(2) Uterne endometrium becomes thick (about 2-3 mm thick), more vascular and more glandular cork-screw shaped. So it prepares itself for implantation.
(3) The epithelium of Fallopian tubes becomes thick and densely ciliated to conduct the ovum / zygote.
(4) Inhibit the secretion of FSH and stimulate the secretion of luteinising hormone (LH) from the anterior pituitary.
(5) Glycogen and fat accumulate in the endometrial cells.
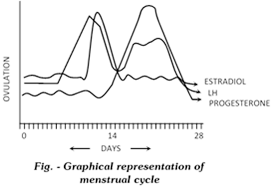
(ii) Ovulatory phase or fertility phase: It involves the ovulation from the Graffian follicle of ovary. The mature graffian follicle rises to the surface of the ovary and ruptures to release ovum. The phenomina is called ovulation. It occurs midway between two menstrual cycles on 14th day of the onset of the menstrual cycle, it is caused by increasing turgidity and contraction of smooth muscles fibres around the Graffian follicle. Ovum is received by the fimbriad of the fallopian tube. Ovum is viable for two days. Ovulation is controlled by the increased level of LH in the blood. Egg at that time is in the secondary oocyte state. LH also starts the change of empty Graffian follicle into corpus luteum and secretion of progesterone from corpus. There is no much change in uterine endometrium during ovulatory phase. In animals the ovulation follow three patterns -
(a) Fix or spontaneous ovulators: In these animals ovulation takes place a fix time in the midway of cycle. There is no need of coitus for ovulation. e.g. Primates (Human, Ape and Monkey)
(b) Induced or reflex ovulators: In these animals copulation or ciotus is necessary for ovulation. e.g. - Rabbit.
(c) Seasonal ovulators: Ovulation occur in breeding season e.g. - Frog.
(iii) Luteal or progestational or Pre-menstrual or Secretory or Post-ovulatory phase: It lasts for about 12 - 14 days and extends from 16th to 28th day of menstrual cycle. It is characterised by following changes -
(a) Corpus luteum (Yellow body): Formed from empty Graffian follicle, increase in size, so is called luteal phase.
(b) Corpus luteum begins to secrete hormone called progesterone. The latter reaches its peak about 22nd day after the beginning of cycle.
(1) Decreases the secretion of FSH and LH (gonadotropins) from anterior pituitary so inhibits the maturation of follicle and ovulation.
(2) Uterine endometrium further proliferates (about 5 mm thick) and is ready for implantation. Uterine glands secrete Uterine milk for the foetus.
(3) Reduces the uterine movements.
In the absence of fertilization, corpus luteum degenerates LH levels falls. Progesterone level is reduced. Reduced level of both progesterone and estrogen causes mensus.
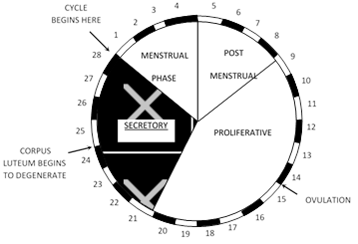
(iv) Menstrual phase or bleeding phase: It lasts for about 3 - 5 days and extends from 1st to 4th day of the menstrual cycle. When the ovum remains unfertilized, then the corpus luteum starts degenerating. The level of progesterone in the blood declines. The uterine tissues fail to be maintained. Then the unfertilized ovum along with ruptured uterine epithelium, about 50 - 100 ml of blood and some mucus is discharged out through the vaginal orifice and is called menstrual flow or menstruation.
Decrease in the level of progesterone and estrogens in the blood stimulates the hypothalamus and anterior pituitary to release FSH-RF and FSH respectively (Positive feedback). FSH starts the follicular phase of next menstrual cycle.
(3) Effect of fertilization: If fertilization occurs and foetus is implanted in the endometrium, the trophoblast cells of the developing placenta secrete a hormone human chorionic gonadotrophin (hCG). This hormone, like LH, maintains the corpus luteum and the secretion of progesterone and estradiol by it. These two hormones check the breakdown of the endometrium of the uterus the absence of menstrual bleeding (the 'period') is the earliest sign of pregnancy. By the 16th week of pregnancy, the placenta produces enough progesterone and estradiol for a normal pregnancy, and the now unnecessary corpus luteum undergoes shrinkage.
(4) Miscarriage: Prematuredegeneration of corpus luteum is the common cause of miscarriage at about 10 – 12 weak of pregnancy (miscarriage means abortion)
(5) Menopause (Climacteric period)
Definition: It is the period when ovulation and menstrual cycle stop in human female.
Period: Between 45 to 55 years. The average period of menopause is currently 52 years. In some, this occurs gradually (in between a period of 1-5 years) while in some this occur abruptly.
Characters: Menopause is characterized by hot flushes (sensation of warmth spreading from the trunk to the face) and a number of psychic symptoms. FSH is secreted in the urine.
Cause: Decline in the estrogen level.
Note: q The function of the testes declines slowly with advancing age, especially in their late 40 yrs or 50 yrs due to decrease in testosterone secretion and is called male climacteric.
(v) Disorders of female reproductive system
(a) Sterility: Inability of the female to conceive, due to inadequacy in structure or function of the genital organs.
(b) Menstrual irregularity
(1) Amenorrhoea: Absence of menstruation.
(2) Hypermenorrhoea: Excessive or prolonged bleeding of uterus.
(3) Dysmenorrhoea: Painful menstruation.
(vi) Pregnancy test: During pregnancy, HCG may be detected in the urine, and this forms the basis of pregnancy test.
Oral contraceptive checks ovulation and implantation (for more information see endocrine system).
You need to login to perform this action.
You will be redirected in
3 sec
