Male Reproductive System
Category : NEET
Male reproductive system
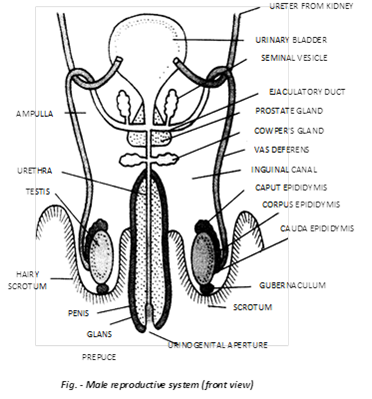
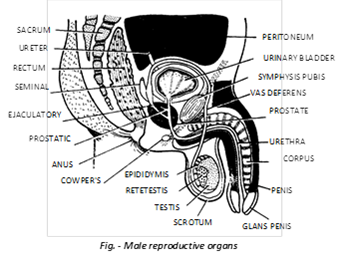
The male reproductive system consists of a scrotum, a pair of testes, vasa efferentia, a pair of epididymis, a pair of vasa deferentia, a pair of ejaculatory ducts, a urethra, a penis and certain glands.
(i) Reproductive organ
(a) Scrotum: The scrotum is a pouch of pigmented skin arising from the lower abdominal wall and hanging between the legs. Its dermis contains almost a continuous layer of smooth muscle fibres called dartos tunic. The scrotum is divided internally into right and left scrotal sacs by a muscular partition, the septum scroti. A scar like raphae marks the position of the septum externally. The testes originate in the abdominal but latter, during the seventh month of development, descend permanently into the respective scrotal sac through passages termed inguinal canal. If an inguinal canal remains open or is torn, a loop of intestine may descent in the scrotum to produce the disorder of inguinal hernia.
Variations in position of testes: In some mammals (lion, bull, horse), the testes remain permanently in the scrotum and keep functioning throughout the year as in man. In certain seasonally breeding mammals, such as bat, otter and llama, (Insectivora, Tubulidentata, chiroptera and most Rodentia) the testes enlarge, become functional, and descent into the scrotum in the breeding season, but thereafter ascent into the abdominal cavity, and become reduced and inactive. In a few cases (elephant, whale, seal) the testes remain permanently in the abdomen as the body temperature is low enough for sperm maturation. Scrotum is absent in such cases. Scrotum is in front of penis in Kangaroo.
(b) Testes: The testes are the primary sex organs. They are about 4 - 5 cm long, 2.5 cm wide and 3 cm thick. They are suspended in the scrotal sacs by spermatic cords.
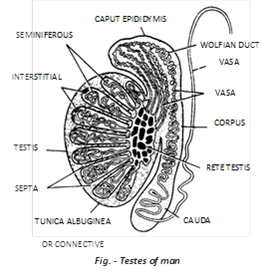
(1) Protective coats (Tunicae): Each testis has three coverings - tunica vaginalis, tunica albuginea and tunica vasculosa. On one side each testis is covered by hollowed tunica vaginalis, a bilayer of peritoneum with a narrow coelomic cavity having coelomic fluid for sliding. The actual covering of testis is a fibrous connective tissue sheath called tunica albuginea. Tunica albuginea also projects inside testis to form a vertical coloumn called mediastinum and a number of transverse septa.
(2) Testicular lobules: In growth of the tunica albuginea, called septa, divide the testis into some 200 to 300 lobules. Each testicular lobule contains 1 - 4 highly convoluted seminiferous tubules, blood vessels and nerve embedded in loose connective tissue. A total of about 1000 seminiferous tubules occur in each testis. Each tubule is about 70 - 80 cm long. In seminiferous tubules lumen develop after puberty. The ends of the seminiferous tubules converge toward the middle of the posterior surface of the testis and join to form short straight tubules called tubuli recti. The tubuli recti open into a network of wider, irregular tubules called rete testis. Here some of the epithelial cells bear a single cilium to aid sperm transport.
Seminiferous tubules: Each seminiferous tubules is lined by germinal epithelium, seminiferous tubules is the site of spermatogenesis. The process occurs in waves along the length of the tubule, taking about 9 weeks (63 days) to complete in man. Seminiferous tubules contain 2 types of cells –
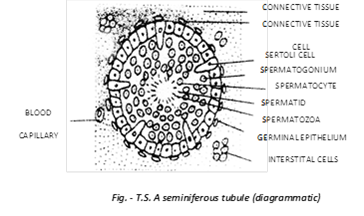
(i) Germ cells: These are spermatogenic cells by mitotic divisions, produce spermatogonia into the lumen of the seminiferous tubule. The spermatogonia grow into primary spermatocytes which undergo meiosis, producing haploid cells, first secondary spermatocytes and then spermatids. Spermatids differentiate by a process of spermiogenesis into dimorphic haploid sperm (containing X or Y chromosome). Mature spermatozoa lie free in the cavity of the seminiferous tubules.
(ii) Somatic cells / Sertoli cells / Sustentacular cells / Nurse cells: These are supportive nutritive and secrete a polypeptide hormone called inhibin and a steroid estradiol which interferes with spermatogenic activity and kinetics of sperm production.
(3) Leydig cells (= Interstitial cell)
(i) These are endocrine cell of testes which lie in the form of clusters or singly in the interstitum (=space between seminiferous tubules).
(ii) They are stimulated by LH (=ICSH) elaborated by luteotroph cells of adenohypophysis which themselves are triggered into activity by LHRH.
(iii) Leydig cells secrete a sex steroids called androgen by using cholesterol. The cells contain a rich repertoire of enzymes which facilitate formation of pathways for steroid biosynthesis and biotransformation. These enzymes are called steroid-dehydrogenases.
(iv) Leydig cells are large, have voluminous eosinophilic cytoplasm, lipid, vacuoles. In humans (but in no other species) they contain elongated cytoplasmic crystals called crystals of Reinke.
(v) Testosterone is the principal androgen. It acts in tandem with FSH to promote spermiogenesis. During pubertal changes it plays a critical anabolic role. It facilitates differentiation of secondary sex characters (change of voice, development of penis, spermatogenic activity, formation of facial hair/beard, pubic and axillary hair, moods, libido etc.)
Rete testis: This is a plexiform arrangement (Network) of space supported by highly vascular collagenous connective tissue. It is lined by cuboidal epithelial cells some of which bear flagella whose activity assists in forward migration of testicular sperm (which are immotile at this stage).
(c) Vasa efferentia: Rete testis is connected to caput epididymis by 12 - 20 fine tubules called vasa efferentia or ductuli efferentes. Their lining epithelium is ciliated for conducting sperms.
(d) Epididymis: On the inner wall of the testis, a highly coiled tubule is present called the epididymis. They are two long (4 - 6 m), narrow (0.4 mm) tubules which lie compacted along the testes from their upper ends to lower back sides.
Epididymes has 3 parts
(e) Vasa deferentia (Singular-vas dererens): The vas deferens is a continuation of the cauda epididymis. It is about 40cm. long and is slightly coiled at first but becomes straight as it enters the abdominal cavity through the inguinal canal. Here, it passes over the urinary bladder, curves round the ureter and joins the duct of a seminal vesicle to form an ejaculatory duct. Near its end, the vas deferens is enlarged to form a spindle-like ampulla for the temporary storage of spermatozoa. At its distal end the ampulla receives a duct from seminal vesicle.
Difference between Vasa efferentia and Vasa deferentia
|
S. No. |
Vasa efferentia |
Vasa deferentia |
|
1. |
Arise from the rete testes. |
Arise from the cauda epididymides. |
|
2. |
Vary from 15 to 20 in number. |
Are only 2 in number? |
|
3. |
Are fine and convoluted |
Are thick slightly coiled in the scrotum, straight in the abdomen |
|
4. |
Lining bears many ciliated cells. |
Lining has sterocilia on many cells. |
|
5. |
Carry spermatozoa from rete testes to caput epididymides |
Carry spermatozoa from cauda epididymides to ejaculatory ducts. |
(f) Ejaculatory ducts: They are short (2 cm) straight muscular tubes each formed by union of a vas deferens and duct of seminal vesicle where ejaculate is formed by mixing of sperms with secretion of seminal vesicle. The two ejaculatory ducts join the urethra within prostate gland.
(g) Urethra: It is the urinary duct leading from the bladder. From the point it is joined by ejaculatory ducts, it carries urine as well as spermatozoa and secretions of the seminal vesicles. It also receives secretion of the prostate and cowper's glands. Urethra is some 20cm long and passes through the penis. The urethra has 4 regions -
(1) Urinary urethra: It carries only urine.
(2) Prostatic urethra: It is a short proximal part which is surrounded by prostate gland.
(3) Membranous urethra: It is a short middle part, without any covering.
(4) Penile urethra: It is a long distal part that passes through the penis.
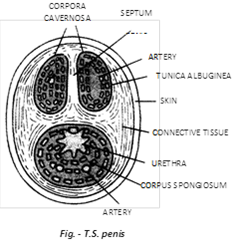
(h) Penis: The penis is an erectile copulatory organ. It consist of a long shaft that enlarges to form an expanded tip, the glans penis. It is covered by a loose, retractable fold of skin, the prepuce or foreskin. Under the skin, the penis contains three columns of erectile tissue: two cylinders of the corpora cavernosa of the penis, placed dorsally, and one cylinder, the corpus spongiosum, along the ventral side. The corpora cavernosa of the penis and the urethra are covered by dense connective tissue, the tunica albuginea. Both urine and semen are carried out of the body through the penis.
Sperm storage: Sperms are stored for the most part in the vasa efferentia, epididymes and proximal parts of vasa deferentia.
(ii) Accessory sex glands: The substances secreted by the accessory, sex glands help in reproduction these are -
(a) Seminal vesicles: The seminal vesicles are long pouches with muscular wall; they secrete spermatozoa activating substances, such as fructose, citrate, inositol, prostaglandins and several proteins, sperms use fructose as a respiratory substrate. Seminal fluid maintains viability and motility of sperms.
Test for rape: Fructose, which is present in the seminal fluid and is not produced anywhere else in the body, provides a forensic test for rape. Its presence in the female's genital tract confirms sexual intercourse.
(b) Prostate gland: The prostate gland surrounds the first portion of the urethra. This gland secretes an alkaline fluid which forms 15 - 30% part of the semen. The secretion nourish and activates the spermatozoa to swim. It is essential for sperm motility (removal causes sterlity).
(c) Cowper's glands: These are also termed as Bulbourethral glands. 1st pair of Cowper's glands are attached to urethra. They secrete alkaline mucus which is discharged into the membranous part of urethra. The mucus lubricates the reproductive tract. This serves to neutralize any acid of urine remaining in the urethra. Secretion of Cowper's glands is produced before the ejaculation of semen.
Secretion of Cowper's glands carries some spermatozoa released before ejaculation. This is one of the reasons for the high failure rate of the withdrawal method of birth control.
(d) Perineal or Rectal glands: These are found both in males and females during the breeding season, these glands secrete and odoriferous liquid which has pheromones or Ectohormones in it. Its smell attracts the animal of opposite sex.
Note: In man, Perineal or Rectal glands are absent.
(e) Other glands: Prepuce contains preputial glands which produce a sebaceous substance which together with desquamated epidermal cells forms a whitish, pasty, foul-smelling accumulation, called smegma, about the base of the glans penis beneath the prepuce.
(iii) Semen: The products of the testes (spermatozoa) and prostate gland, alongwith fluid from the seminal vesicle, are collectively knows as semen. Release of spermatozoa from urethra is known as ejaculation.
A person with a sperm count below 20 million will be physiologically sterlile. Fusion of defective sperm (e.g. 22+xy) with ovum causes many birth defects e.g. klinefelter's syndrome.
(iv) Hormonal control of male reproductive system: The growth, maintenance and functions of secondary sex organs (epididymis, vasa deferentia, accessory glands and penis) are under the control of testosterone hormone secreted by Leydig's cells of testis, while those of seminiferous tubules and Leydig's cells are controlled by Follicular Stimulating Hormone (FSH) and Interstitial Cells Stimulating Hormone (ICSH) of anterior pituitary lobe respectively.
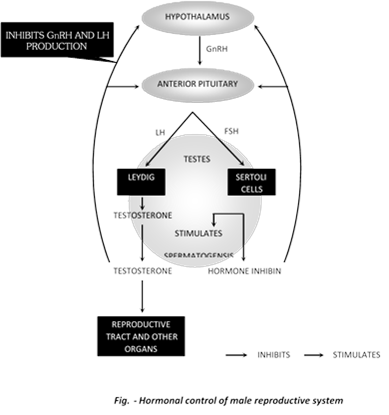
Sertoli cells also secretes two proteins
(a) Androgen Binding Protein (ABP) that concenterates testosterone in the seminiferous tubules.
(b) (Inhibin) protein which suppress FSH secretion. Release of FSH, LH or ICSH, in turn, are controlled by release of hypothalamic gonadotropin releasing hormone (GnRH).
(v) Onset of puberty in the male: Puberty is the period when reproductive organs become functional. It is triggered by the secretion of the hormone testosterone in the testes. This hormone brings about growth and maturation of the secondary sex organs and development of the accessory sex characters. The latter induce -
(a) Enlargement of the penis and scrotum.
(b) Broadening of the shoulders.
(c) Growth of body and facial hairs.
(d) Deepening of the voice duce enlargement of layrnx and thickening of vocal-cords.
(e) Increased development of musculature and bones.
(f) Increase in height so characteristic of male puberty.
(vi) Male sex act: The male sex act involves 3 phases: erection of the penis, copulation (often called sexual intercourse in humans) and subsidence of erection.
(a) Erection: Erection of the penis is caused by rush of arterial blood into the empty sinuses of its spongy tissue on sexual excitement. As the spongy tissue distends, it compress the veins, inhibiting the flow of blood out of the tissue. Filling of tissue with blood is called vasocongenstion. Erection makes the penis long and stiff for entry into the female's vagina for copulation. Stiffness is due entirely to the hydraulic pressure of blood filling the sinuses.
(b) Copulation: Mucus from the urethral glands, Cowper's glands and vaginal glands provides lubrication for copulation. Friction due to rhythmic movements of sexual intercourse stimulate the sensory cells of the glans penis. This stimulation releases semen into the proximal part of urethra by contraction of reproductive glands and ducts. This process is called emission. Then the rhythmic, wavelike contractions of the muscles at the base of the penis cause forceful discharge, called ejaculation, of semen into the vagina. One ejaculate (about 3 ml.) contains 200 to 400 million spermatozoa. Ejaculation marks the climax of copulation.
Orgasm: At the peak of sexual stimulation, pleasurable sensation, called orgasm, occurs. It usually last only a few seconds.
(c) Subsidence of erection: After ejaculation, the arterioles to the penis contract, reducing the blood flow to the penis, and erection subsides. This often takes a few minutes.
(vii) Movement of spermatozoa to site of fertilization: In the female genital tract, alkalinity of the semen helps neutrilize acidity in the vagina. This protects the sperms and increase their motility, prostaglandins of the semen thin the mucus at the opening of the uterus, and also stimulate contractions of the uterine muscles. These contractions help the semen move up the uterus called syring absorption mechanism. When ejaculated, the semen first coagulates, making it easier for uterine contractions to push up; and is then liquefied by the anticoagulating enzymes, enabling the sperms to start swimming in the uterus. From here, they reach the oviduct. In the oviduct, the spermatozoa are capacitated (attain the ability to penetrate the ovum). Somewhere in the ampulla of the oviduct, an ovum, if present, may be fertilized by a sperm, and procreation of the special starts.
(viii) Disorders of male reproductive system: Only a few are mentioned.
(a) Prostatomegaly (Prostatic hypertrophy): This is enlargement of prostate gland. If often occurs in old age. The enlarged gland may block the urethra, causing frequent night urination (nocturia) or difficult or painful micturition. Prostate cancer is very common in men. It is treated surgically or with drugs.
(b) Impotence: This is inability of the male to achieve and or maintain erection of the penis long enough to engage in or complete copulation.
(c) Sterility: Inability of the male's sperm to fertilized the ovum, it may or may not be associated with impotence. Sterlity also results from immobility and morphological abnormality of the sperms, and from low sperm count in the semen.
You need to login to perform this action.
You will be redirected in
3 sec
