Skeletal Tissue
Category : NEET
Skeletal Tissue
It provide support and surface for attachment of muscle. Skeletal connective tissue form the frame work of body.
It provide rigidity to body. These protect the various organ and help in locomotion. It is of three types.
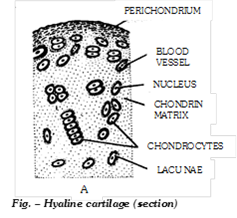
(i) Cartilage: Cartilage is a solid but semi-rigid and flexible connective tissue. Cartilage is a nonvascular connective tissue, consisting of cells embeded in a resilent matrix of chondrin. Chondrin is a protein of cartilage. Cartilage differs from other connective tissue in that only one cell type the chondrocytes is present; Chondrocytes are found in small opening called lacunae. Chondroblast, a cartilage forming cells are embeded in firm, translucent matrix younger cartilage are possesing phagocytic cells called chondroclasts which eats up extra matrix of cartilage to provide new shape to the cartilage. It is a vascular so, nutrient must reach by process of diffusion movement is through the matrix from blood vessels located in a specialized connective tissue membrane called perichondrium, a outer covering of cartilage. Regeneration of cartilage can occur from its peri-chondrium. Cartilage is said to be metabolically nearly inactive. In kids the cartilage cells show 2 types of growth.
(a) Types of cartilage: It is of following types -
(1) Hyaline cartilage: It is most primitive and glass like cartilage. Its matrix is transparent homogenous and pearly white or bluish green in colour, contain chondrin. When the chondrocytes or cartilage cells are arranged in groups of two, four etc. in a single lacuna it is called a cell nest. It is slightly elastic and also known as articular cartilage because it forms the articular surface of joints. Hyaline cartilage is found in trachea, larynx and bronchi, limb bones (called hyaline cap), sternum, in the hyoid apparatus nasal septum, ribs (sternal parts) larynx (cricoid, thyroid), nasal cartilage (nasal septum).
(2) Fibro cartilage (White fibrous cartilage): In this cartilage, the small amount of matrix of cartilage is packed with large number of bundles of thick white (collagen) fibres. So it is toughest and less flexible. Between the bundles of white fibres, there are scattered lacunae, each containing a chondrocyte. It is found in intervertebral discs and acts as shock absorber. It is also found in pubic symphysis and helps in parturition (child birth). The intervertebral discs remain contracted when the body is active, but relaxed when the body is at rest. That is why, our body becomes a bit taller during sleep and after death.
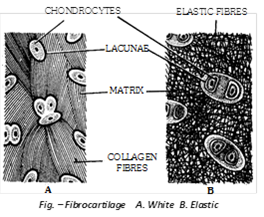
(3) Elastic cartilage (Yellow elastic cartilage): In this cartilage, the matrix is packed with yellow or elastic fibres which run in all directions to form a network. It appears yellow and opaque. The chondrocytes are present in lacunae between the yellow fibres. Owing to the presence of yellow fibres, it is very flexible. It gives recoiling power to structures. It is found in mammalian pinna, pharyngotympanic tube, epiglottis, some laryngeal and bronchiolar cartilages.
(4) Calcified cartilage: It is modified hyaline cartilage, It is hard and non elastic due to deposition of calcium salt-hydroxy appetite in matrix. It is found in pubis of old frog, supra-scapula of frog, quadrate cartilage of frog., shark vertebrae, in man ends of long bone, head of humerus and femur. Calcification may also occur as a regular growth process of bone due to age. It reduces elasticity of the cartilage and makes it more rigid.
Differences between Bone and Cartilage
|
Bone |
Cartilage |
|
1. Matrix is composed of a tough, inflexible material, the ossein. |
1. Matrix is composed of a firm, but flexible material, the chondrin. |
|
2. Matrix is always impregnated with calcium salts. |
2. Matrix may be free or impregenated with calcium salts. |
|
3. Bone cells lie in lucunae singly. |
3. Cartilage cells lie in lacunae singly or in groups of two or four. |
|
4. Osteocytes are irregular and give off branching processes in the developing bone. |
4. Chondroblasts are oval and devoid of processes. |
|
5. Lacunae give off canaliculi. |
5. Lacunae lack canaliculi. |
|
6. There are outer and inner layers of special bone forming cells, the osteoblasts, that produce new osteocytes, which secrete new lamellae of matrix. |
6. There are no special cartilage-forming cells. Cartilage grows by division of all chondroblasts. |
|
7. Matrix occurs largely in concentric lamellae. |
7. Matrix occurs in a homogenous mass. |
|
8. Bone is highly vascular. |
8. Cartilage in nonvascular. |
|
9. Bone may have bone marrow at the centre. |
9. No such tissue is present. |
(ii) Bone: Bone is a highly calcified (mineralized), hard and rigid connective tissue. It is the major component of adult vertebrate endoskeleton. Besides its mechanical function of supporting the body architecture and internal organs as a frame work, of protecting delicate organ like brain, heart, etc. of forming to muscles to facilitate movement and locomotion, the bone is also a metabolically dynamic tissue which functions as a homeostatic reservoir of ions of calcium, magnesium, phosphorous, etc. About 97% of total calcium of body occurs in the endoskeleton.
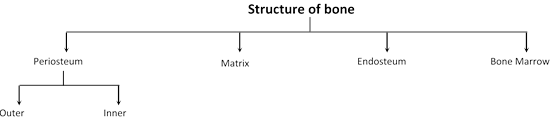
(a) Periosteum: It is a membrane that forms an envelop around the bone. Periosteum is comprises of two distinct layers. Outer layer consist of thin white fibrous connective tissue. Inner layer consist of osteoblasts, osteoblasts are spider like bone cells, also known as bone forming cells, because they produces new bone materials.
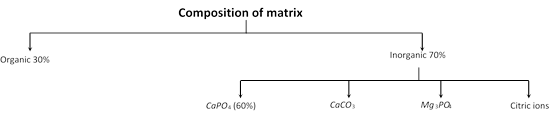
(b) Matrix: Matrix is composed of protein called ossein. The matrix forms thin plates called lamellae. Lamellae are of three types. Haversian lamellae (occur around Haversian canal) concentric or circumferential lamellae (inner to periosteum and outer to endosteum) and interstitial, lamellae (between Haversian system). In the lamellae minute bone cells osteocytes are present.
(c) Endosteum: It is present outer to the bone marrow cavity. Endosteum is a membrane which lines the marrow cavity. It is comprises of two distinct layers, one is of fibrous connective tissue and another is osteoblasts.
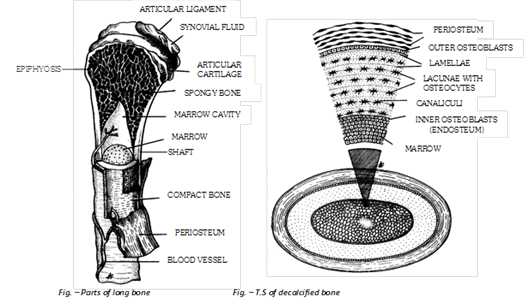
(d) Bone marrow: Bone marrow is a specialized type of soft, diffuse connective tissue called “Myeloid tissue”. It takes part in production of blood cells hence known as haemopoietic tissue. It is composed of adipose tissue, areolar tissue and blood. It is of two types -
(1) Red bone marrow: Red in colour due to presence of lot of blood vessels. In foetal life and at birth present in entire skeleton. After 5th year red bone marrow replaced by yellow bone marrow, at 20-25 years red bone marrow present at ribs, sternum, clavicles, vertebrae, scapula, pelvis, epiphysis of humerus and femur. Produces RBCs, WBC, monocytes, eosinophils and platelets.
(2) Yellow bone marrow: Yellow in colour and has much fatty tissue (adipose tissue), present in shaft of long bones. Produces blood cells in emergency i.e. at the time of excessive loss of blood, yellow bone marrow may be replaced by red bone marrow in anaemia.
(e) Haversian system: A haversian canal, its lamellae and osteocytes form a haversian system. Haversian canals are found in bone matrix of long bone, like humerus of mammals. Haversian canals contain artery and veins, osteoblasts in areolar tissue, nerves and lymph. It is also called osteon.
(f) Types of bone cells: Three types of cells are found in bone:
(1) Osteoblast: Bone forming cells found in all bone surfaces. It is small cells synthesize and secrete osteoid, an important part of ground substance. Process of osteoblast is called canaliculi.
(2) Osteocyte: Mature, nondividing osteoblast surrounded by matrix, lying within lacunae.
(3) Osteoclast: Bone destroying cells take part in resorption of bones, contain large amount of acid phosphatase enzyme. 4-Osteoprogenitor.
(g) Types of bone
(1) On the basis of their texture: The bones are divided into two categories spongy or cancellous or tubecular bones and compact or periosteal bones.
Differences between Spongy bone and Compact bone.
|
Characters |
Spongy bone |
Compact bone |
|
Arrangement of lamellae |
There is no regular Haversian system so have spongy texture. |
Have regular Haversian system |
|
Occurrence |
In skull bones, ribs, centrum of vertebrae and epiphyses of long bones |
In the shaft (diaphysis) of long bones |
|
Marrow cavity |
Broad |
Narrow |
|
Type of bone marrow |
Red marrow in the spaces between lamellae |
Yellow marrow in marrow cavity |
|
Function |
Marrow forms RBCs and Granular WBCs |
Marrow stores fats |
(2) On the basis of origin of bone: Ossification or osteogenesis is the process of bone formation. A bones are classified into four categories.
Differences between Cartilaginous, Dermal, Sesamoid and Visceral bones
|
Cartilaginous (Endochondrial) bone |
Dermal (Intramembranous) bone |
Sesamoid bone |
Visceral bone |
|
These are formed by ossification directly on the cartilages and formation involves deposition of body matter by osteoblasts and resorption by osteoclast. |
These are formed by ossification in the dermis of the skin. |
These are formed by ossification at the joints of the bones or on the tendon and ligament. |
They are formed in the soft organs. |
|
These are elongated and hard bones Examples: Vertebrae, humerus, femur and fibula. |
These are membrane-like bones. Examples: skull bones, phalanges, clavicles. |
These are small sized disc like bones. Example: patella bone (knee cap). |
Examples: oscordis, ospenis, osclitoris. |
(3) On the basis of treatment: These are of two types
Differences between Dried bone and Decalcified bone
|
Characters |
Dried bone |
Decalcified bone |
|
Type of treatment |
Subjected to high temperature. |
Subjected to dilute solution of HCl. |
|
Nature of matter left |
With only mineral matter. |
With only organic matter. |
|
Marrow cavity |
Empty. |
With bone-marrow. |
|
Fate of cells |
Periosteum, endosteum, osteoblasts and osteocytes are absent being killed by high temperature. |
Periosteum, endosteum, osteoblasts and osteocytes all are present. |
|
Lacunae |
Lacunae present. |
Lacunae absent. |
(h) Functions of bone:
(1) Support: Bones form the framework of the body and contribute to the shape, alignment and positioning of the body.
(2) Protection: Bony “boxes” protect the delicate structures they enclose,
(3) Movement: Bones with their joints constitute levers that move as muscle contract.
(4) Mineral storage: Bones are the major reservoir for calcium, phosphorus and other minerals.
(5) Haematopoiesis: Blood cell formation is carried out by myeloid tissue.
(iii) Notochord: It is found in all chordate, It is replaced by vertebral column in vertebrate. Notochord is rod like structure. Notochord is made up of chordal cells.
(iv) Structure of frog’s bone: A typical long bone of an adult vertebrate, such as a limb bone (humerus, femur, etc.), is distinguishable into the long, middle, cylindrical shaft (diaphysis) and the roughly spherical articular heads (Epiphyses). The shaft is hollow. Its cavity, called marrow or medullary cavity, is filled with a soft and semisolid fatty neurovascular tissue, yellow bone narrow. The latter is yellow in middle part of the shaft, but red due to abundant blood vessels towards the epiphysis. In mammals the, red bone marrow contains erythroblast cells which form red blood corpuscles. A thin single layered epithelium called endosteum, lines the marrow cavity. Cells of endosteum are young, unbranched and some what flattened bone cells, called osteoblast, which secrete the osteoid matrix or ossein of the bone when active. The ossein is deposited towards outer side in concentric rings called lamellae (lamellar bone). The middle line of each lamella is marked by an angular ring of lacunae. Each lacuna encloses a branched mature bone cell (osteocyte). As new lamellae are laid down by endosteum, its osteoblasts also divide and form the lacunar rings of the lamellar matrix. Thus the role of endosteum is to add to the thickness of the bone from its inner side. The endosteum also contains bone reabsorbing cells called osteoclast. A thick and tough sheath, called periosteum, forms an envelope around the bone. It comprises two distinct layers - a thin outer layer of dense fibrous connective tissue with fibroblast and a thin inner layer of osteoblast like those of endosteum.
(v) Structure of mammalian long bone: Mammalian bones are quite different and complicated in structure than those of frog and other vertebrates. Since mammals have attained larger body size in evolution, their bones are thicker and stronger. Osteocytes of deep seated lacunae in those bones become cut off from the vascular supply of periosteum and bone marrow. Hence, mammalian bones have a wide spread network of vascular supply embedded in their matrix. Within the matrix of the compact bone of the shaft of a long mammalian bone, such as humerus, femur, tibia, etc., blood vessels are lodged in a matrix of slender branching canals. The main canals, called Haversian canals, usually run parallel to the long axis of a bone. Numerous transverse and oblique Volkmann’s canals connect the haversian canals with each other and with the marrow cavity and periosteum. Haversian canals or ventral canals or central canals are possessing nerve, lymphatics, blood vessels (either artery or vein or both otherwise capillary only), areolar tissue, bone marrow. To provide the osteocytes with maximum facility of chemical exchange, the matrix of compact mammalian bones is laid down in a very orderly but highly complicated system of lamellae. On basis of the arrangement of the lamellae, such a bone can be divided into 4 zones:
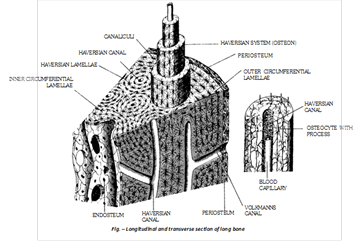
(a) Zone of Haversian systems or Osteons: Four to twenty concentric rings of lamellae surround each haversian canal, establishing a cylindrical unit of bone structure, called “Haversian system or Osteon”. The major, medullary part of the bone is formed of osteons (osteonal bone). All lacunae of an osteon communicate with their own haversian canal by means of canaliculi. Hence, the osteocytes of these lacunae carry their chemical exchange with the blood vessel lodged in this haversian canal.
(b) Interstitial zone: Since remodelling of bone in some bones continues throughout life, osteons are continuously reabsorbed and formed again and again. The narrow gaps, left between completed osteons are, therefore, remnants of former lamellae or osteons. These are irregular and called interstitial lamellae.
(c) Outer circumferential zone: This is the thin peripheral zone of compact bone between haversian zone and periosteum. Lamellae of bone matrix in this zone run parallel to the long axis of the bone.
(d) Inner circumferential zone: This is the thin zone of bone between haversian zone and endosteum. This also comprises longitudinal lamellae. Osteocytes of outer and inner circumferential zones communicate with the blood vessels, respectively of periosteum and bone marrow. Haversian systems are absent in spongy bone of mammals.
(vi) Formation and growth of bone: The process of bone-formation is called osteogenesis or ossification. It is a 2-phased process - first the special organic matrix is laid down by osteoblasts and then, follows its mineralization or calcification. Bone formation starts in foetal life in second month. It produce four types of bones with regard to their source.
(a) Endochondral ossification: Most bones of the body are more or less elongated. These are all cartilaginous bones formed by endochondral osteogenesis. Each such bone replaces an elongated, rod like embryonic model of hyaline cartilage which is usually completely destroyed during osteogenesis. The cartilaginous model is covered by a functional perichondrium and it continues growing even during its ossification. Before the onset of ossification, the cartilaginous model undergoes some regional differentiation of its tissue -
(1) Cartilage cells (chondrocytes) at the centre of diaphysis become large and vacuolated. Their lacunae also become large. The cartilage matrix (chondrin) between these lacunae becomes calcified. This is now the primary centre of ossification. Its chondrocytes gradually die and disintegrate.
(2) The perichondrial sheath around the central diaphysial region of the cartilage differentiates into bone sheath or periosteum; cells of its inner layer become osteogenic, i.e., osteoblasts.
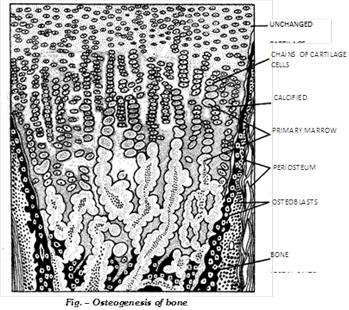
(3) Buds containing blood vessels and overlying osteoblasts now grow inwards from the periosteum and erode their way into the primary center of ossification. Destruction of the calcified cartilage during the erosion is perhaps performed by certain large, multinucleate and phagocytic bone-eating cells called osteoclasts. The latter are probably formed by fusion of several osteoblasts which have assumed bone eroding function. Due to irregular erosion, narrow strips or bars of original calcified cartilage are left here and there, and original lacunae form an irregular system of intercommunicating medullary spaces, called primary marrow cavities. Branches of blood vessels and osteoblasts fill up the spaces in the form of an embryonic bone marrow.Now ossification begins at two sites. The osteoblasts of periosteum lay down a “periosteal collar” of compact bone around the middle region of the cartilage mode. Simultaneously, the osteoblasts of embryonic marrow become arranged in linear series and start ossification around the cartilage bars, forming bone trabeculae of a primary spongy bone. Both of these sites of ossification progressively thicken and extend towards both ends of the cartilage model. Osteoblasts, which are entrapped within the bone matrix, become branched osteocytes. The spaces, these cells occupy in the matrix, become branched lacunae. Owing to a continuous process of bone remodelling i.e., bone-eating or reabsorption by osteoclasts and bone - laying by osteoblasts. Most of the bony trabeculae in axial part of shaft region are removed. Hence, a continuous marrow cavity, lined by endosteum, is formed. Later, new (secondary) centres of ossification establish in the terminal (epiphysial) parts of the cartilage model. Hence, spongy bone is laid down in these parts. Eventually, the entire cartilage model, except thin articular surfaces at the two ends, is replaced by bone. That is why, bones formed in this way are called cartilage or replacing bones. All bones of limbs, girdles (except clavicles) and vertebral column, and some of the skull are cartilage bones.
(b) Intramembranous ossification: This type of ossification occurs, not in a prior cartilage model, but in collagenous connective tissue membranes beneath embroyonic skin. It begins at certain fixed centres which are marked by profuse capillary networks. Fibroblasts in these centres differentiate into osteoblasts which cluster around the respective capillary network and start forming osteoid bone around themselves. Mineralization of osteoid bone begins. Some osteoblasts become completely surrounded by bone. These thus become osteocytes in lacunae. Other osteoblasts remain closely applied to the surfaces of the bone. These proliferate, spread over the first-formed bone and continue osteogenesis. The latter is more rapid at certain points than at others. This results in formation of spongy bone. While spongy bone is, thus, formed around the centre of ossification, the surround cells of periosteum are potentially osteogenic. These lay down a covering sheet of compact bone upon the surface. Typical dipolic bones are formed in this way. These become invested upon original cartilaginous box of skull and at some other cartilages, giving these strength and protection. These are, therefore, also called investing bones. All flat bones of cranium, facial skeleton, clavicles of pectoral girdles and terminal phalanges are investing bones. By continued remodelling, some of these may completely change into compact bones.
(c) Intratendinous ossification: These bones are formed by the ossification of tendons (white collagen tissue). e.g. - Patella (knee cap) present at knee joint and pisiform (pea shaped) present in wrist. Tendinous bones are called sesamoid bones.
Important Tips
You need to login to perform this action.
You will be redirected in
3 sec
